Chronic Obstructive Pulmonary Disease (COPD)
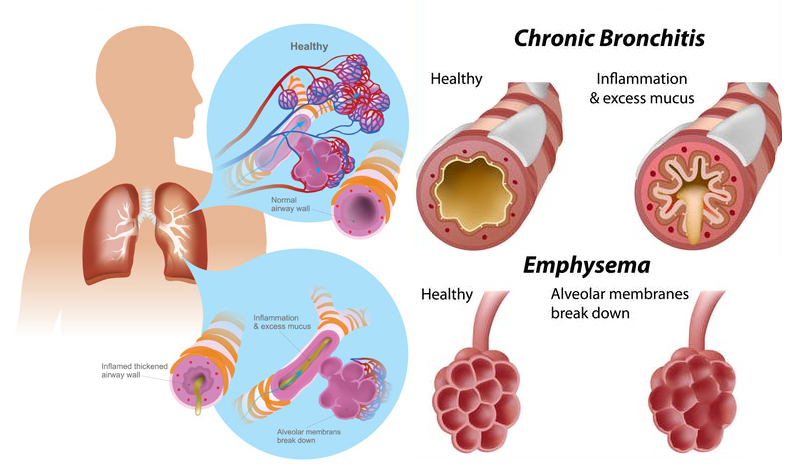
Chronic obstructive pulmonary disease (COPD) is a progressive life threatening lung disease characterized by chronic obstruction of lung airflow that interferes with normal breathing and is not fully reversible and also that causes breathlessness (initially with exertion) and predisposes to exacerbations & serious illness. The most common conditions are emphysema and chronic bronchitis. Many people with COPD have both of these conditions. Emphysema slowly destroys air sacs in your lungs, which interferes with outward air flow. Bronchitis causes inflammation and narrowing of the bronchial tubes, which allows mucus to build up.
Emphysema and chronic bronchitis are the two most common conditions that contribute to COPD. These two conditions usually occur together and can vary in severity among individuals with COPD. Chronic bronchitis is inflammation of the lining of the bronchial tubes, which carry air to and from the air sacs (alveoli) of the lungs. It's characterized by daily cough and mucus (sputum) production. Emphysema is a condition in which the alveoli at the end of the smallest air passages (bronchioles) of the lungs are destroyed as a result of damaging exposure to cigarette smoke and other irritating gases and particulate matter.
Common symptoms include breathing difficulty, cough, mucus (sputum) production and wheezing. It's typically caused by long-term exposure to irritating gases or particulate matter, most often from cigarette smoke. People with COPD are at increased risk of developing heart disease, lung cancer and a variety of other conditions. Although COPD is a progressive disease that gets worse over time, COPD is treatable but not curable. With proper management, most people with COPD can achieve good symptom control and quality of life, as well as reduced risk of other associated conditions.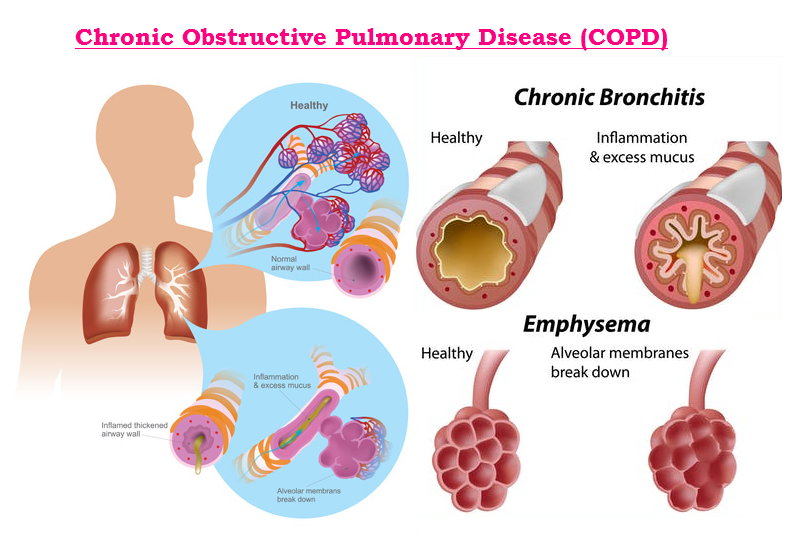
Chronic obstructive pulmonary disease (COPD) is a major cause of morbidity and mortality across the globe. According to World Health Organization estimates, 65 million people have moderate to severe COPD. More than 3 million people died of COPD in 2005 corresponding to 5% of all deaths globally and it is estimated to be the third leading cause of death by 2030.
Most of the information available on COPD prevalence, morbidity and mortality comes from high-income countries. Even in those countries, accurate epidemiologic data on COPD are difficult and expensive to collect. However, it is known that low- and middle-income countries already shoulder much of the burden of COPD with almost 90% of COPD deaths taking place in these countries. In this issue of Lung India, the joint ICS/NCCP (I) consensus guidelines for the diagnosis and management of COPD have been published to facilitate the Indian practitioner in burden reduction, diagnosis and management of COPD.
In 2015, 3.2 million people died from COPD worldwide, an increase of 11.6 percent compared with 1990. During that same time period, the prevalence of COPD increased by 44.2 percent to 174.5 million individuals. In the United States, an estimated 16 million adults have COPD. However, that may be an underestimate. The American Lung Association (ALA) thinks there may be as many as 24 million American adults living with COPD. Rates of COPD are highest in the Southeast and Midwest states. In 2015, the rate was as low as 3.8 percent in only one state — Utah. In West Virginia, the highest, it was 12 percent.
COPD was the fourth-leading cause of death in the United States in 2016, following heart disease, cancer, and unintentional injuries. Worldwide, COPD was previously more common in men but the disease now affects men and women equally. In the United States, women are still 37 percent more likely to have COPD than men. More than 7 million U.S. women have COPD, and millions more are believed to have symptoms, yet haven’t been diagnosed.
Developing countries are changing fast. Socio-economic development, industrialization, urbanization, changing age structure, and changing lifestyles have the countries at a position where they are facing an ever increasing burden of Non-communicable diseases (NCD). In India NCDs were estimated to have accounted for 53% of all deaths and 44% of disability-adjusted life-years (DALYs) lost in 2005. Of these chronic respiratory disease accounted for 7% deaths and 3% DALYs lost.
India also has had the ignominy of experiencing the “highest loss in potentially productive years of life” worldwide in 2005. Crude estimates suggest there are 30 million COPD patients in India. India contributes a significant and growing percentage of COPD mortality which is estimated to be amongst the highest in the world; i.e. more than 64.7 estimated age standardized death rate per 100,000 amongst both sexes. This would translate to about 556,000 in case of India (>20%) out of a world total of 2,748,000 annually. Such mammoth volumes of disease have the potential to overwhelm health systems and state economies.
Causes & Risk Factors of COPD :
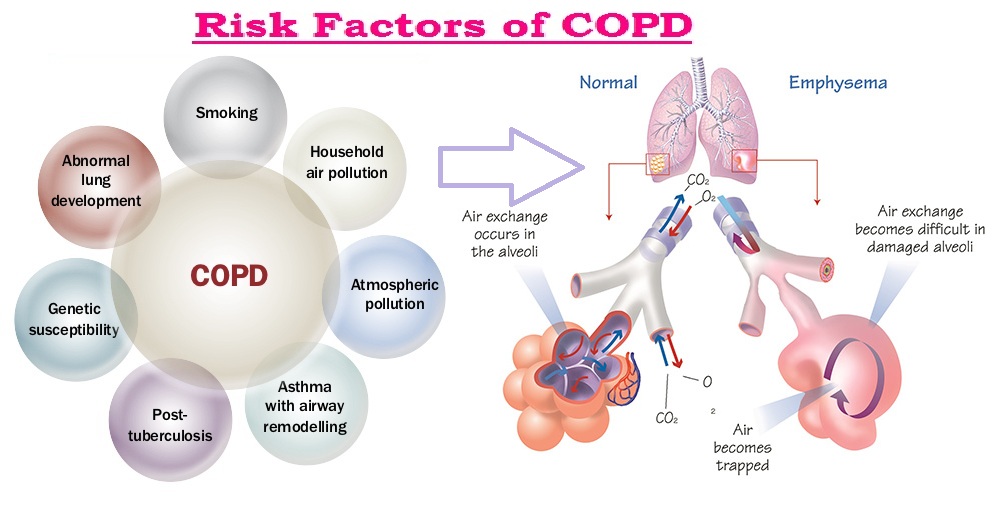
Most cases of COPD are associated with long-term exposure to harmful substances by inhaling pollutants; that includes active smoking (cigarettes, pipes, cigars, etc.), and Passive smoking. Fumes, chemicals and dust found in many work environments are contributing factors for many individuals who develop COPD. Genetics factor can also play a role in an individual’s development of COPD—even if the person has never smoked or has ever been exposed to strong lung irritants in the workplace. Here is more information on the top three risk factors for developing COPD:
- Smoking : The harmful chemicals in smoke can damage the lining of the lungs and airways. COPD most often occurs in people 40 years of age and older who have a history of smoking. These may be individuals who are current or former smokers. While not everybody who smokes gets COPD, most of the individuals who have COPD (about 90% of them) have smoked. Some research also suggests that being exposed to other people's cigarette smoke (passive smoking) may increase your risk of COPD.
- Environmental Factors : Chronic obstructive pulmonary disease (COPD) can also occur in those who have had long-term contact with harmful pollutants in the workplace. Some of these harmful lung irritants include certain chemicals, dust or fumes (cadmium dust and fumes, grain and flour dust, silica dust, welding fumes, isocyanates, coal dust etc.). Heavy or long-term contact with secondhand smoke or other lung irritants in the home, such as organic cooking fuel, may also cause COPD. Exposure to air pollution over a long period can affect the lungs work and could increase the risk of COPD.
- Genetic Factors : Even if an individual has never smoked or been exposed to pollutants for an extended period of time, they can still develop COPD. Around 1 in 100 people with COPD has a genetic tendency to develop the condition, called alpha-1-antitrypsin deficiency. Alpha-1 Antitrypsin Deficiency (AATD) is the most commonly known genetic risk factor for emphysema2. Alpha-1 Antitrypsin related COPD is caused by a deficiency of the Alpha-1 Antitrypsin protein in the bloodstream. Without the Alpha-1 Antitrypsin protein, white blood cells begin to harm the lungs and lung deterioration occurs. The World Health Organization and the American Thoracic Society recommends that every individual diagnosed with COPD be tested for Alpha-1.
Sign & Symptoms of COPD :
Chronic obstructive pulmonary disease (COPD) makes breathing increasingly more difficult, chronic cough and sputum production. It's develops slowly and usually becomes apparent after 40 or 50 years of age. But it develops slowly over many years and the patient may not be aware he/she have it at first. Most people with COPD do not have any noticeable symptoms until they reach their late stage.
Symptoms may be mild at first, beginning with intermittent coughing and shortness of breath. As it progresses, symptoms can become more constant to where it can become increasingly difficult to breathe. Some people with COPD have acute exacerbations, which are flare-ups of severe symptoms.
Common symptoms of COPD include:
- Increasing breathlessness – this may only happen when exercising at first, and the person may sometimes wake up at night feeling breathless.
- A persistent chesty cough with phlegm that does not go away.
- Frequent chest infections.
- Persistent wheezing.
- Frequent coughing (with and without sputum).
- Tightness in the chest.
- Frequent colds, Flu or other respiratory infections.
- Lack of energy etc.
The symptoms will usually get gradually worse over time and make daily activities increasingly difficult, although treatment can help slow the progression. Sometimes there may be periods when symptoms get suddenly worse – known as a flare-up or exacerbation. It's common to have a few flare-ups a year, particularly during the winter.
 Less common symptoms of COPD include:
Less common symptoms of COPD include:
- Weight loss
- Fatigue
- Tiredness
- Swollen ankles from a build-up of fluid (edema)
- Chest pain and coughing up blood – although these are usually signs of another condition, such as a chest infection or possibly lung cancer.
These additional symptoms only tend to happen when COPD reaches an advanced stage.
Complication of COPD :
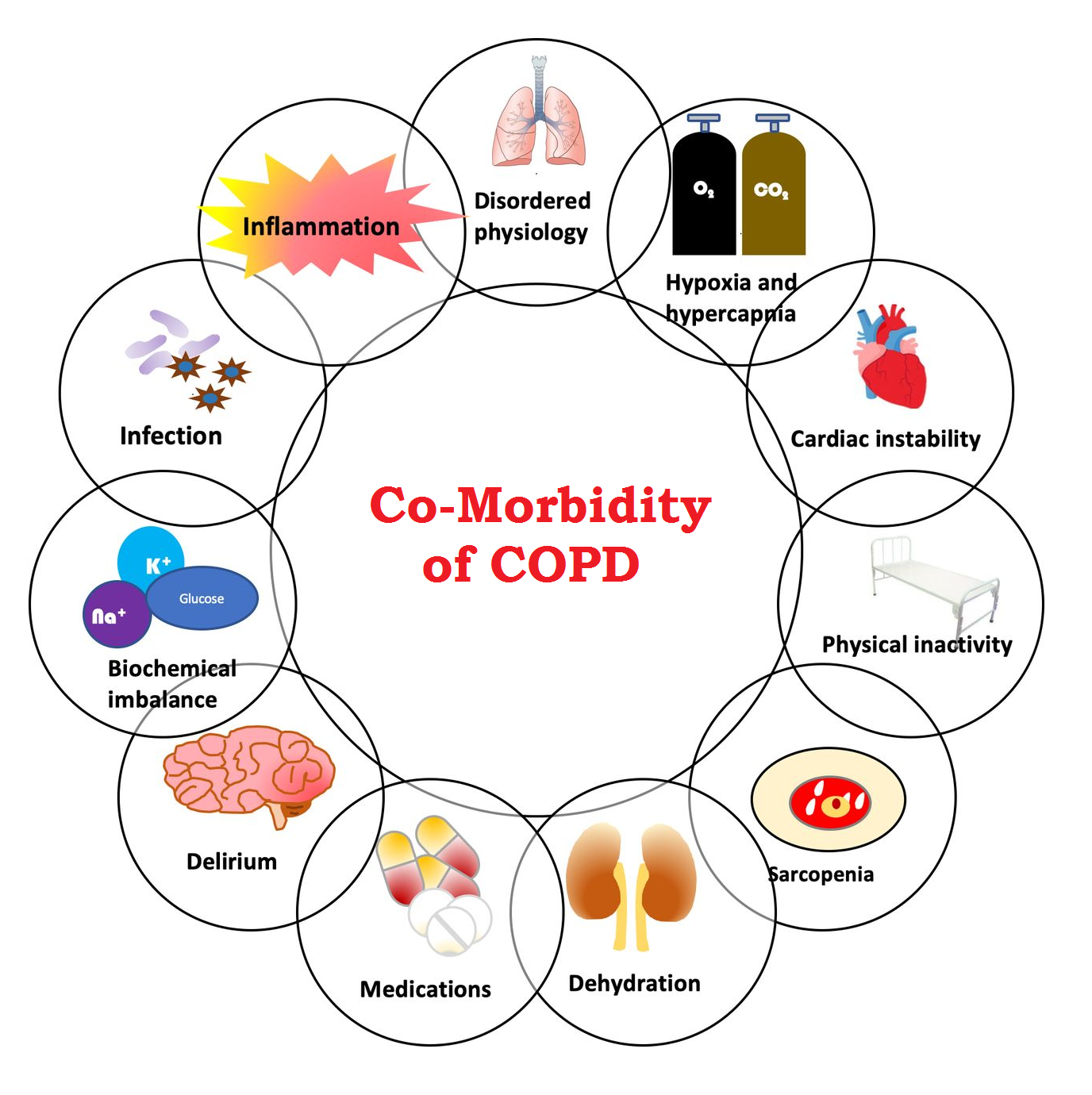
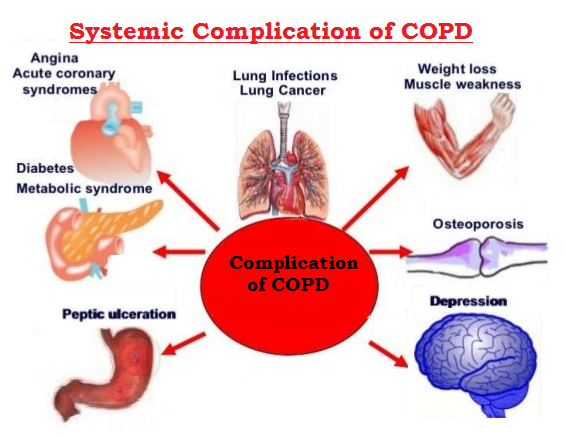
Chronic obstructive pulmonary disease (COPD) can cause many complications, including:
- Respiratory infections : People with COPD are more likely to catch colds, the flu and pneumonia. Any respiratory infection can make it much more difficult to breathe and could cause further damage to lung tissue.
- Collapsed Lung (Pneumothorax) : COPD can damage lung tissue. And if air leaks into the space between a lung and chest wall, that lung can collapse like a deflated balloon. Patient might have sudden shortness of breath, feel sharp chest pain or tightness, or have a hacking cough. Treatments range from extra oxygen to surgery. To help prevent a collapsed lung from happening, stop smoking and consult with doctor regularly.
- Poor Gas Exchange : Blood carries oxygen to cells throughout body and carbon dioxide away from them. But because patient're not breathing in and out fully, may have less oxygen than need or more carbon dioxide than want in the blood. Either of these may be why patient have shortness of breath. A high carbon dioxide level can also give a headache and make patient woozy.
- Heart problems : For reasons that aren't fully understood, COPD can increase risk of heart disease, including heart attack.
- Lung cancer : People with COPD have a higher risk of developing lung cancer.
- High blood pressure in lung arteries : COPD may cause high blood pressure in the arteries that bring blood to your lungs (pulmonary hypertension).
- Thinning Bones (Osteoporosis) : It's common for people with COPD to get osteoporosis. They've often been smokers, they take steroids, it's hard for them to get enough bone-strengthening exercise, and they can be low on bone-building vitamin D. Brittle, weak bones break more easily. And a break will sideline from activity. Protect bones with weight-bearing exercise like walking and strength training with stretchy bands. Doctor may want to check bone density with the painless X-ray test called a DEXA scan. They might want the patient to take calcium and vitamin D supplements or possibly bone-building drugs.
- Depression & Anxiety : Difficulty breathing can keep you from doing activities that you enjoy. And dealing with serious illness can contribute to the development of depression.
Diagnosis of COPD :
There’s no single test for the diagnosis of Chronic obstructive pulmonary disease (COPD). Diagnosis is based on symptoms, a physical exam, and diagnostic test results. During the physical exam, doctor will use a stethoscope to listen to lungs breathe. Based on all this information, doctor may order some of the following tests to get a more complete picture:
- Medical history and physical exam : These will give doctor important information about patient health as like patient is a smoker or have smoked in the past, exposed to lung irritants on the job, exposed to a lot of secondhand or passive smoke, a family history of COPD, asthma or other respiratory conditions or and take over-the-counter or prescription medications.
- Lung function tests : Lung function tests, including an FEV1 test. These tests measure the amount of air in the lungs and the speed at which air moves in and out. Spirometry - a most important noninvasive test to assess lung function that measures how much and how quickly a person can forcibly exhale air. A Peak flow test - a breathing test that measures how fast patient can blow air out of his/her lungs, which can help rule out asthma.
- Chest X-ray : This helps rule out other conditions with similar symptoms of COPD, such as Chest infection or lung cancer etc.
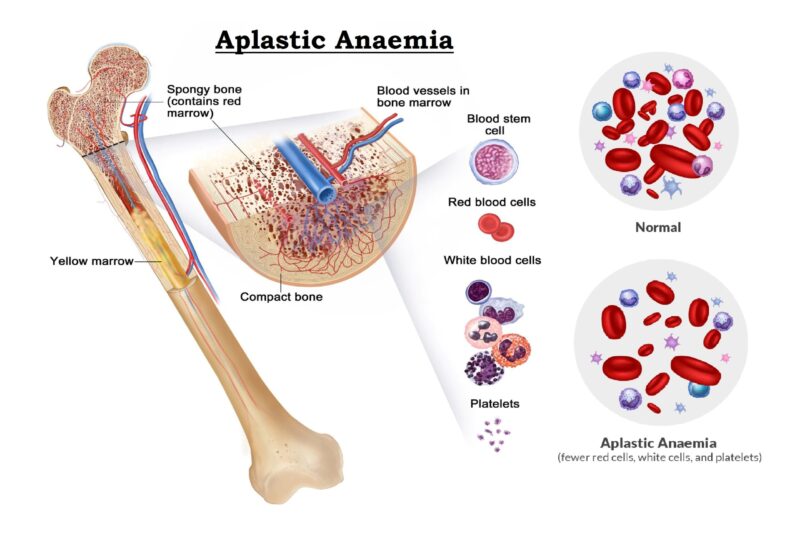
- Blood test : This helps rule out other conditions with similar symptoms of COPD, such as anaemia, polycythaemia, acute or chronic infection etc.
- Sputum Examination : A sputum sample of the patient may be tested to check for signs of a chest infection.
Special tests done as needed. - Arterial blood gas test : This test measures how much oxygen, carbon dioxide and acid is in the blood. It helps doctor to decide whether patient need oxygen treatment.
- Oximetry : This test measures the oxygen saturation in the blood. It can be useful in finding out whether oxygen treatment is needed, but it provides less information than the arterial blood gas test.
- Electrocardiogram (ECG) or Echocardiogram : These tests may find certain heart problems that can cause shortness of breath.
- Transfer factor for Carbon monoxide : This test looks at whether your lungs have been damaged, and if so, how much damage there is and how bad COPD might be.
- Alpha-1 antitrypsin (AAT) test : AAT is a protein patient body makes that helps protect the lungs. People whose bodies don't make enough AAT are more likely to get emphysema.
- A CT scan : This gives doctors a detailed picture of the lungs.
Treatment of COPD :
Chronic obstructive pulmonary disease is not curable. However, available medical and physical treatments can help relieve symptoms, improve exercise capacity and quality of life and reduce the risk of death. The most effective and cost-effective available treatment for COPD in people who continue to smoke is smoking cessation. Smoking cessation can slow down the progress of the disease in smokers and decrease COPD-related deaths. In some, but not all, people with COPD, treatment with inhaled corticosteroid medicines has a beneficial effect.
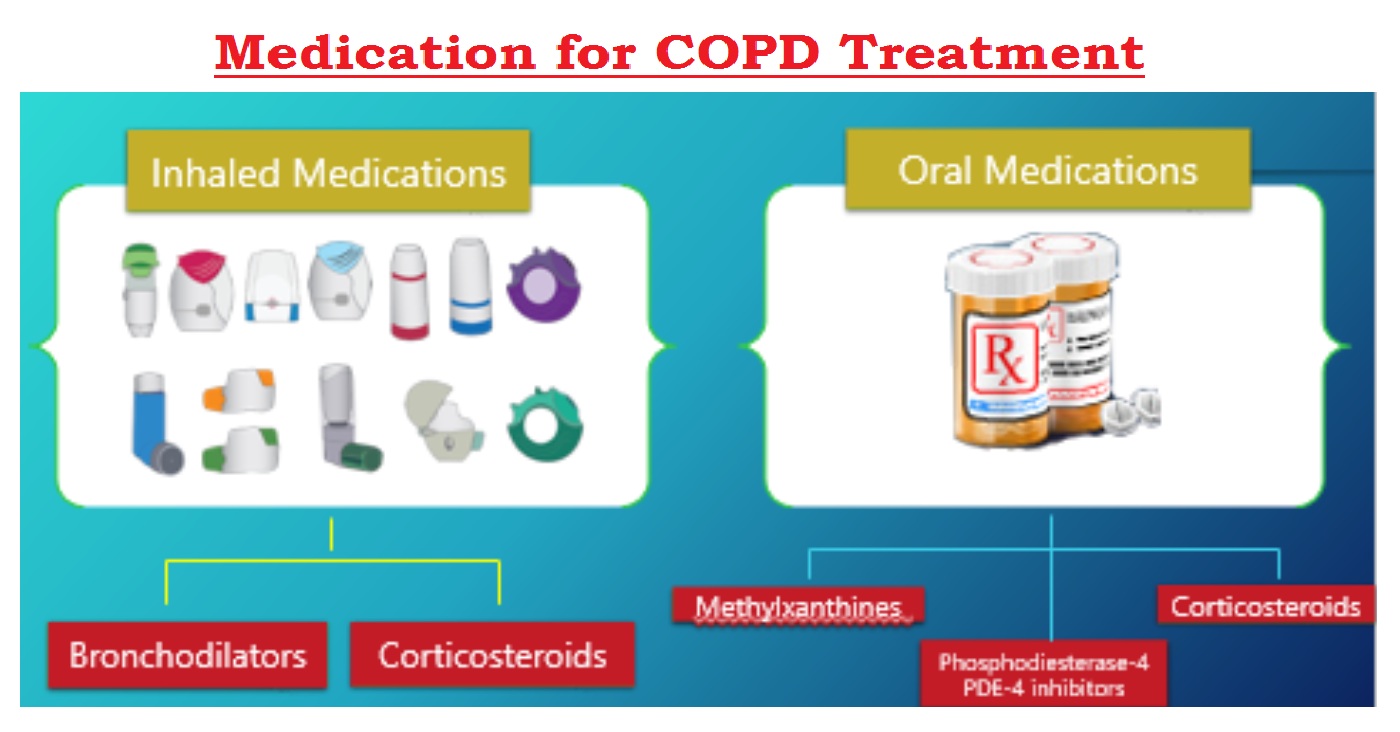
Much of the treatment for COPD includes things patient can do for himself. Quitting smoking is the most important thing patient can do to slow the disease and improve his/her quality of life. The medicines used to treat COPD can be long-acting to help prevent symptoms or short-acting to help relieve them. The medications most commonly used to control COPD include:
1. Inhalers
If COPD is affecting breathing, Patient will usually be given an inhaler. This is a device that delivers medicine directly into lungs as he/she breathe in. A doctor will advise on how to use an inhaler correctly and how often to use it. There are several different types of inhaler for COPD. The main types include:
- Short-acting bronchodilator inhalers : For most people with COPD, short-acting bronchodilator inhalers are the first treatment used. Bronchodilators are medicines that make breathing easier by relaxing and widening respiratory airways. There are 2 types of short-acting bronchodilator inhaler:
- Beta-2 agonist inhalers – such as salbutamol and terbutaline.
- Antimuscarinic inhalers – such as ipratropium
Short-acting inhalers should be used when feel breathless, up to a maximum of 4 times a day.
- Long-acting bronchodilator inhalers : If patient experience symptoms regularly throughout the day, a long-acting bronchodilator inhaler will be recommended. These work in a similar way to short-acting bronchodilators, but each dose lasts for at least 12 hours, so they only need to be used once or twice a day. There are 2 types of long-acting bronchodilator inhaler:
- Beta-2 agonist inhalers- such as salmeterol, formoterol and indacaterol.
- Antimuscarinic inhalers- such as tiotropium, glycopyronium and aclidinium
Some new inhalers contain a combination of a long-acting beta-2 agonist and antimuscarinic.
- Steroid inhalers : If patient are still becoming breathless when using a long-acting inhaler, or he/she have frequent flare-ups (exacerbations), a physician may suggest including a steroid inhaler as part of treatment. Steroid inhalers contain corticosteroid medicines, which can help to reduce the inflammation in airways.
Steroid inhalers are normally prescribed as part of a combination inhaler that also includes a long-acting medicine.
2. Tablets
If your symptoms are not controlled with inhalers, a doctor may recommend taking tablets or capsules as well.
- Theophylline : Theophylline is a type of bronchodilator. It's unclear exactly how theophylline works, but it seems to reduce swelling (inflammation) in the airways and relax the muscles lining them. Theophylline comes as tablets or capsules and is usually taken twice a day.
- Mucolytics : If patient have a persistent chesty cough with lots of thick phlegm, the doctor may recommend taking a mucolytic medicine called carbocisteine. Mucolytic medicines make the phlegm in throat thinner and easier to cough up. Carbocisteine comes as tablets or capsules and is usually taken 3 or 4 times a day. If carbocisteine does not help or cannot take it for medical reasons, another mucolytic medicine called acetylcysteine is available. This comes as a powder that patient can mix with water. Acetylcysteine powder has an unpleasant smell, like rotten eggs, but this smell should go away once mix it with the water.
- Steroid : If patient have a particularly bad flare-up, may be prescribed a short course of steroid tablets to reduce the inflammation in airways. A 5-day course of treatment is usually recommended, as long-term use of steroid tablets can cause troublesome side effects such as weight gain, mood swings and weakened bones (osteoporosis). Longer courses of steroid tablets must be prescribed by a COPD specialist.
- Antibiotics : Doctor may prescribe a short course of antibiotics if you have signs of a chest infection, such as becoming more breathless, coughing more and or noticing a change in the color (such as becoming brown, green or yellow) and/or consistency of phlegm (such as becoming thicker) Sometimes patient may be given a course of antibiotics to keep at home and take as soon as experience symptoms of an infection.
3. Pulmonary Rehabilitation :
Pulmonary rehabilitation is a specialised programme of exercise and education designed to help people with lung problems such as COPD. It can help improve how much exercise patient are able to do before feel out of breath, as well as symptoms, self-confidence and emotional wellbeing. Pulmonary rehabilitation programmes usually involve 2 or more group sessions a week for at least 6 weeks. A typical programme includes:
- Physical exercise training tailored to patient needs and ability – such as walking, cycling and strength exercises.
- Education about patient's condition for him and his/her family.
- Dietary advice
- Psychological and emotional support
The programmes are provided by a number of different healthcare professionals, including physiotherapists, nurse specialists and dietitians.
4. Other treatments :
If patient have severe symptoms or experience a particularly bad flare-up, he/she may sometimes need additional treatment.
- Nebulised medicine : Nebulised medicine may be used in severe cases of COPD if inhalers have not worked. This is where a machine is used to turn liquid medicine into a fine mist that patient breathe in through a mouthpiece or a face mask. It enables a large dose of medicine to be taken in one go. shown how to use it.
- Roflumilast : Roflumilast is a new medicine that can be used to treat flare-ups. It is recommended for people whose symptoms have suddenly become worse at least 2 times over the past 12 months, and who are already using inhalers. Roflumilast comes as tablets and the medicine helps reduce inflammation inside the lungs and airways.
- Long-term oxygen therapy : If COPD causes a low level of oxygen in blood, patient may be advised to have oxygen at home through nasal tubes or a mask. This can help stop the level of oxygen in the blood stream becoming dangerously low, although it's not a treatment for the main symptoms of COPD, such as breathlessness. Long-term oxygen treatment should be used for at least 16 hours a day.
The tubes from the machine are long, so patient will be able to move around the home. Portable oxygen tanks are available if need to use oxygen away from home. - Ambulatory oxygen therapy : Some people with COPD will benefit from ambulatory oxygen, which is oxygen you use when you walk or are active in other ways. If your blood oxygen levels are normal while you're resting but fall when you exercise, you may be able to have ambulatory oxygen therapy rather than long-term oxygen therapy.
- Non-invasive ventilation (NIV) : If patient are taken to hospital because of a bad flare-up, may have a treatment called non-invasive ventilation (NIV). This is where a portable machine connected to a mask that covers patient nose or face is used to support his/her lungs and make breathing easier.
5. Surgery
Surgery is usually only suitable for a small number of people with severe COPD whose symptoms are not controlled with medicine. It is rarely used for COPD patients.
There are 3 main operations that can be done:
- Bullectomy – An operation to remove a pocket of air from one of the lungs, allowing the lungs to work better and make breathing more comfortable.
- Lung volume reduction surgery – An operation to remove a badly damaged section of lung to allow the healthier parts to work better and make breathing more comfortable.
- Lung transplant – An operation to remove and replace a damaged lung with a healthy lung from a donor
These are major operations done under general anaesthetic, where patient are asleep, and involve significant risks.
Prevention of COPD :
Unlike some diseases, Chronic obstructive pulmonary disease (COPD) typically has a clear cause and a clear path of prevention, and there are ways to slow the progression of the disease. The majority of cases are directly related to smoking, and the best way to prevent COPD is to never smoke — or to stop smoking now. If patient are a longtime smoker, these simple statements may not seem so simple, especially if patient have tried quitting - once, twice or many times before. But keep trying to quit. It's critical to find a tobacco cessation program that can help quit for good. It's patient best chance for reducing damage of lungs.
Occupational exposure to chemical fumes and dusts is another risk factor for COPD. If patient work with these types of lung irritants, talk to supervisor about the best ways to protect himself, such as using respiratory protective equipment.
Here are some steps can take to help prevent complications associated with COPD:
- Quit smoking to help reduce risk of heart disease and lung cancer.
- Get an annual flu vaccination and regular vaccination against pneumococcal pneumonia to reduce risk of or prevent some infections.
- Talk to doctor if feel sad or helpless or think that may be experiencing depression.
Stopping smoking is especially important if anyone have low levels of the protein alpha-1 antitrypsin. People who have an alpha-1 antitrypsin deficiency may lower their risk for severe COPD if they get regular shots of alpha-1 antitrypsin.


This article is a source of inspiration, I recommend it.
Thanks and keep it up!