Celiac Disease : Sign & Symptoms, Risk Factors, Diagnosis, Complications, Treatment & Prevention
Celiac disease is a hereditary genetic autoimmune disorder where the ingestion of gluten leads to damage in the small intestine. It is estimated to affect 1 in 100 people worldwide. The prevalence of celiac disease was 4% in South America, 0.5% in Africa and North America, 0.6% in Asia, and 0.8% in Europe and Oceania. According to experts at the All India Institute of Medical Sciences, New Delhi Celiac disease affects close to six to eight million people in India. Celiac disease must not be confused with gluten allergy or its intolerance. It is a kind of an autoimmune disorder occurring in people who are genetically predisposed. Maximum cases are undiagnosed and are at risk for long-term health complications.
Celiac disease is hereditary, meaning that it runs in families. People with a first-degree relative with celiac disease (parent, child, sibling) have a 1 in 10 risk of developing celiac disease. Celiac disease is also known as Coeliac disease, Celiac sprue, Non-tropical sprue, and Gluten sensitive enteropathy.
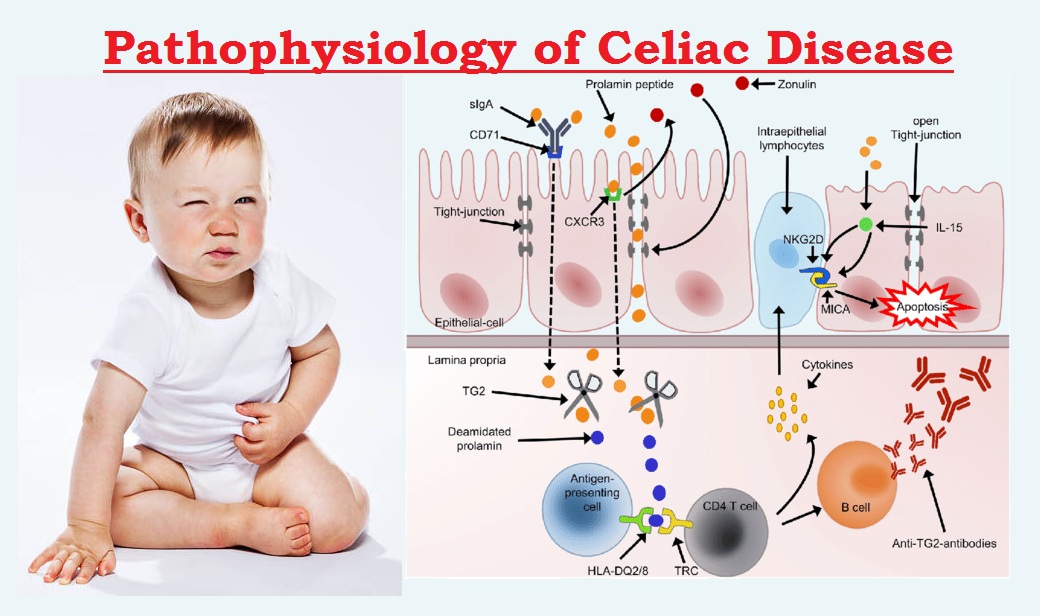
Celiac disease occurs from an interaction between genes, eating foods with gluten and other environmental factors, but the precise cause isn't known. Infant feeding practices, gastrointestinal infections and gut bacteria might contribute to developing celiac disease.
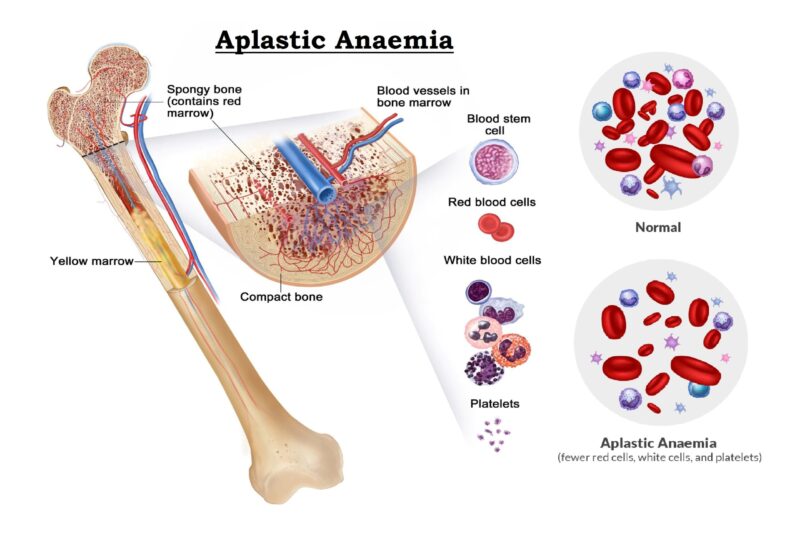
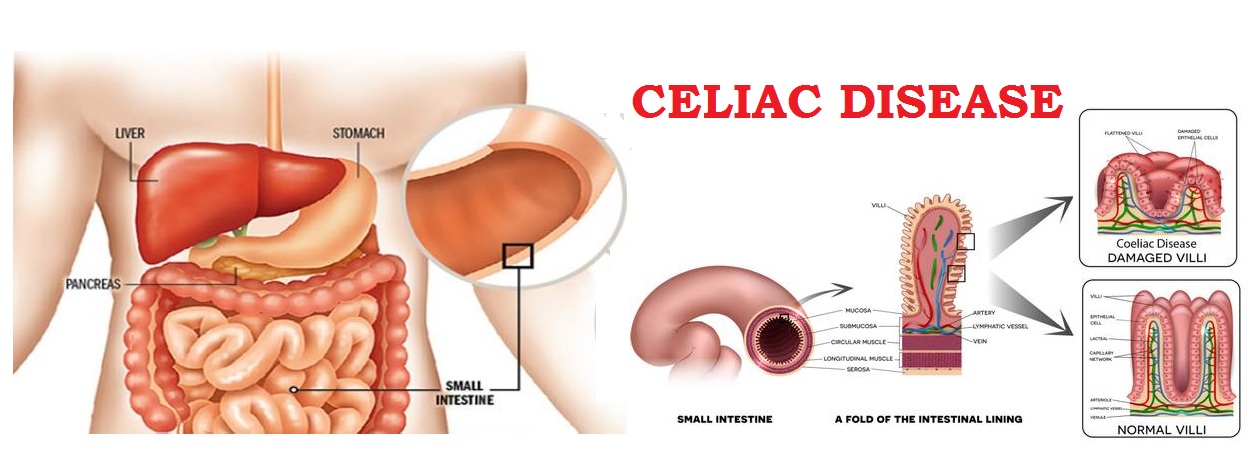
Sometimes celiac disease is triggered - or becomes active for the first time - after surgery, pregnancy, childbirth, viral infection or severe emotional stress. When the body's immune system overreacts to gluten in food, the reaction damages the tiny, hair-like projections (villi) that line the small intestine. Villi absorb vitamins, minerals and other nutrients from the food you eat. If your villi are damaged, you can't get enough nutrients, no matter how much you eat.
Some gene variations appear to increase the risk of developing the disease. But having those gene variants doesn't mean you'll get celiac disease, which suggests that additional factors must be involved. The rate of celiac disease in Western countries is estimated at about 1 percent of the population. Celiac disease is most common in Caucasians; however, it is now being diagnosed among many ethnic groups and is being found globally.
Sign & Symptoms
The signs and symptoms of celiac disease can vary greatly and are different in children and adults. The most common signs for adults are diarrhea, fatigue and weight loss. Adults may also experience bloating and gas, abdominal pain, nausea, constipation, and vomiting. However, more than half of adults with celiac disease have signs and symptoms that are not related to the digestive system, including:
-
- Anemia, usually resulting from iron deficiency.
- Loss of bone density (osteoporosis) or softening of bone (osteomalacia).
- Itchy, blistery skin rash (dermatitis herpetiformis).
- Damage to dental enamel.
- Mouth ulcers.
- Headaches and fatigue.
- Nervous system injury, including numbness and tingling in the feet and hands, possible problems with balance, and cognitive impairment.
- Joint pain.
- Reduced functioning of the spleen (hyposplenism).
- Acid reflux and heartburn.
- Children
In Children under 2 years old, typical signs and symptoms of celiac disease include:
-
- Vomiting.
- Chronic diarrhea.
- Swollen belly.
- Failure to thrive.
- Poor appetite.
- Muscle wasting.
Older Children may experience:
-
- Diarrhea
- Constipation
- Weight loss
- Irritability
- Short stature
- Delayed puberty
- Neurological symptoms, including attention-deficit/hyperactivity disorder (ADHD), learning disabilities, headaches, lack of muscle coordination and seizures
Risk Factors
Celiac disease can affect anyone. However, it tends to be more common in people who have:
Diagnosis
Researchers estimate that only 20 percent of people with celiac disease may receive a diagnosis.
-
- Doctors may order two blood tests to help diagnose celiac disease.
- Serology testing looks for antibodies in your blood. Elevated levels of certain antibody proteins indicate an immune reaction to gluten.
- Genetic testing for human leukocyte antigens (HLA-DQ2 and HLA-DQ8) can be used to rule out celiac disease.
- If the results of these tests indicate celiac disease, your doctor may order an endoscopy to view your small intestine and to take a small tissue sample (biopsy) to analyze for damage to the villi.
- It's important to be tested for celiac disease before trying a gluten-free diet. Eliminating gluten from your diet may change the results of blood tests so that they appear to be normal.
Complications
Untreated, celiac disease can cause:
-
- Malnutrition : The damage to your small intestine means it can't absorb enough nutrients. Malnutrition can lead to anemia and weight loss. In children, malnutrition can cause slow growth and short stature.
- Loss of calcium and bone density : Malabsorption of calcium and vitamin D may lead to a softening of the bone (osteomalacia or rickets) in children and a loss of bone density (osteoporosis) in adults.
- Infertility and miscarriage : Malabsorption of calcium and vitamin D can contribute to reproductive issues.
- Lactose intolerance : Damage to your small intestine may cause you to experience abdominal pain and diarrhea after eating lactose-containing dairy products, even though they don't contain gluten. Once your intestine has healed, you may be able to tolerate dairy products again. However, some people continue to experience lactose intolerance despite successful management of celiac disease.
- Cancer : People with celiac disease who don't maintain a gluten-free diet have a greater risk of developing several forms of cancer, including intestinal lymphoma and small bowel cancer.
- Neurological problems : Some people with celiac disease may develop neurological problems such as seizures or peripheral neuropathy (disease of the nerves that lead to the hands and feet).
- In children, celiac disease can also lead to failure to thrive, delayed puberty, weight loss, irritability and dental enamel defects, anemia, arthritis, and epilepsy
Treatment
A strict, lifelong gluten-free diet is the only way to manage celiac disease. In addition to wheat, foods that contain gluten include:
-
- Barley
- Bulgur
- Durum
- Farina
- Graham flour
- Malt
- Rye
- Semolina
- Spelt (a form of wheat)
- Triticale
Doctor may refer to a Dietitian, who can help the patient & plan a healthy gluten-free diet.
Once remove gluten from the diet, inflammation in the small intestine generally begins to lessen - usually within several weeks, though the patient may start to feel better in just a few days. Complete healing and regrowth of the villi may take several months to several years. Healing in the small intestine tends to occur more quickly in children than adults. If the patient accidentally eat a product that contains gluten, he/she may experience abdominal pain and diarrhea. Some people experience no signs or symptoms after eating gluten, but this doesn't mean it's not harmful to them. Even trace amounts of gluten in his/her diet can be damaging, whether or not they cause signs or symptoms. Hidden gluten can be present in foods, medications and nonfood products, including:
-
- Modified food starch, preservatives and food stabilizers.
- Prescription and over-the-counter medications.
- Vitamin and mineral supplements.
- Herbal and nutritional supplements.
- Lipstick products
- Toothpaste and mouthwash
- Envelope and stamp glue.
- Play-Doh
Vitamin and mineral supplements : If nutritional deficiencies are severe, Doctor or dietitian may recommend taking vitamin and mineral supplements. Patient may need to supplement levels of:
-
- Calcium
- Folate
- Iron
- Vitamin B-12
- Vitamin D
- Vitamin K
- Zinc
Vitamins and supplements are usually taken in pill form. If digestive tract has trouble absorbing vitamins, doctor may give them by injection. Patient need to be sure that the vitamins and supplements are gluten-free.
Prevention
Celiac disease can't be prevented. If the patient already have celiac disease, can prevent symptoms-and damage of small intestine-by eating a gluten-free diet. Celiac Disease - Eating a Gluten-Free Diet. Some adults with celiac disease have a poorly functioning or nonfunctional spleen, which is a risk factor for developing a pneumococcal infection. For this reason, Doctor may recommend that patient get immunized with the pneumococcal vaccine.


Very great post. I just stumbled upon your weblog and wanted to say that I have really loved browsing your blog posts. After all I will be subscribing to your website and I am hoping you write once more soon!
Like!! I blog frequently and I really thank you for your content. The article has truly peaked my interest.