Cerebrospinal Fluid (CSF) : Significance, Function, Collection, Patient preparation, Complication & Laboratory analysis
Cerebrospinal fluid (CSF) is a clear and colorless fluid that surrounds the brain and spinal cord with a density ranging from 1.003 to 1.008 which allows the brain to “float” in the fluid. It supplies nutrients to the tissues of the Central nervous system and helps to protect the brain and spinal cord from injury.
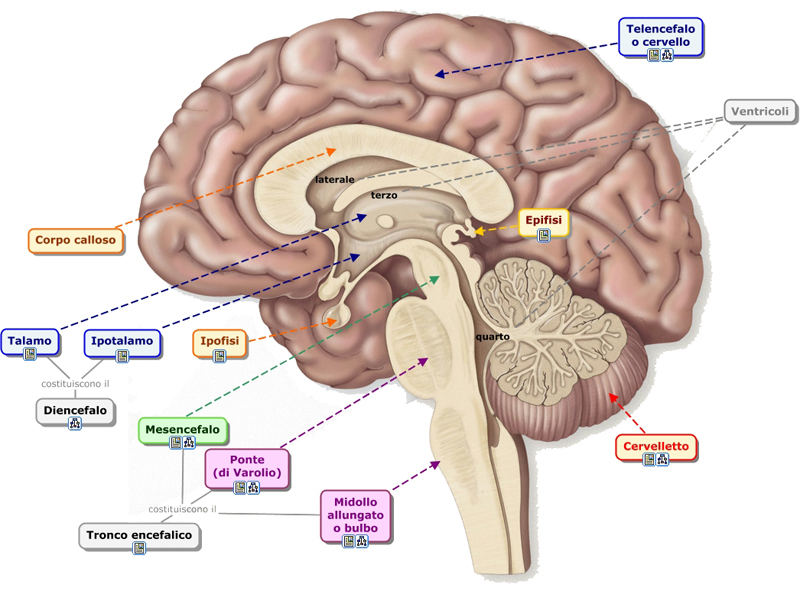
Compared to plasma, CSF has a lower concentration of glucose, protein, and potassium while having a higher concentration of chloride. The volume of the CSF in adults is 100–150 ml. The volume is less in children and varies according to the body length. About two-third part of CSF is secreted by the Choroid plexus of the four ventricle. The remaining part of CSF are secreted by the Ependymal surfaces of the ventricles and the Arachnoid mater. A small amount of CSF also comes from the blood flow in the brain.
http://medicoinfo.org/cerebrospinal-fluid-csf-significance-function-collection-patient-preparation-complication-laboratory-analysis/
CSF is produce by an active process where Sodium ions are transported across the Epithelial cells and pushed outside of the Choroid plexus. The positive Sodium ions then attract negative Chloride ions. This changes the osmotic gradient and the CSF with the higher ion concentration draws water across the Choroid plexus membrane (osmosis). Glucose, Bicarbonate ions and Sodium are then transported out of the blood capillaries by other processes. This brings the composition of CSF similar to that of plasma, although the quantities of chloride ions, potassium ions and glucose are lower in the CSF.
Fluid secreted from the Choroid plexus of the lateral passes through the first and third ventricles and into the fourth ventricle. Minute amounts of CSF are added to the bulk from the lateral ventricles in the third and fourth ventricle. By exiting the fourth ventricle through the two lateral foramina and the midline foramen, the Cerebrospinal fluid enters the Cisterna magna. This then drains into the Subarachnoid space which surrounds the entire brain and Spinal cord. Eventually CSF flows through the Arachnoidal villi and is emptied into the several venous sinuses of the Cerebrum. It is then returned into the venous circulation.
Function of Cerebrospinal fluid (CSF)
The main function of the Cerebrospinal fluid is to act as a shock absorber thereby cushioning the brain. There is a very slight difference in the specific gravity of the brain and CSF which allows the brain to be “suspended” in the CSF. With a moderate blow or sudden jerking of the neck and head, the brain will move with the skull and not collide with it. With more severe blows, however, the brain can collide with the skull on the side opposite to the impact though the impact is usually reduced significantly due to the presence of CSF.
Brain tissue is delicate and the brain is a heavy organ. By being suspended in CSF, it is not weighed down against the bony skull which could damage the lower parts of the brain tissue. Alterations in the volume of CSF is a compensatory mechanism to deal with raised intracranial pressure associated with a Haemorrhage, Haematoma or Cerebral edema. Since the brain lacks a true lymphatic system, excess protein in the brain tissue spaces are carried through the Perivascular spaces and into the Subarachoid spaces by the Cerebrospinal fluid. By passing through the Arachnoid villi, the CSF carries the protein back into the venous blood stream. This route via the Perivascular spaces may also be utilized to flush out cellular debris in the brain following an infection and other metabolic wastes.
Significant Features of Cerebrospinal fluid :
Pressure:
- Increased:
- Brain Tumor.
- Meningitis, Enccephalitis.
- Neurosyphilis.
- Subarachnoid and Intracerebral hemorrhage.
- Hypertensive Encephalopathy.
- Venous sinus Thrombophlebitis.
- Hydrocephalus.
- Benign raised Intracranial tension.
- Uremia
- Emphysema.
- Decreased:
- Repeat L.P. soon after the brain tumor.
- Subarachnoid spinal block.
- Subdural hematoma.
Appearance :
- Turbid: Pyogenic meningitis.
- Cobweb: T.B. meningitis.
- Blood tinged:
- Subarachnoid hemorrhage.
- Trauma to spinal blood vessels.
- Bleeding diathesis.
- Xanthochromia (Yellow tinting of the C.S.F.).
- Following hemorrhage in the C.S.F.
- High protein content of the C.S.F (Guillain Barre syndrome, spinal block, neurofibroma, etc.).
- Jaundice.
- Tumors near the cauda equina,around the ventricles and acoustic neuroma.
Proteins :
- Increased:
- Meningitis.
- Encephalitis including Poliomyelitis.
- Disseminated sclerosis.
- Guillain Barre Syndrome.
- Neurosyphilis.
- Spinal cord compression.
- Intra- cranial tumor.
- Cerebral arteriousclerosis.
- Decreased: ( Not known)
Glucose :
- Increased:
- Diabetes mellitus.
- Following I.V. glucose administration.
- Encephalitis.
- Decreased: Meningitis.
Chiorides :
- Increased : (Not known)
- Decreased :
- Purulent and Tuberculous meningitis.
- Systemic hypochloremia.
Cells :
- Polymorphonuclear leucocytosis :
- Pyogenic meningitis.
- Acute syphilitic meningitis.
- Actute poliomyelities (early stage).
- Epidural abscess.
- Lymphocytosis :
- Meningitis - tuberculous, viral, syphilitic & late stage of pyogenic.
- Encephalitis.
- Poliomyelitis- later stages.
- Disseminated sclerosis.
- Cerebral tumor.
- Cortical venuous thrombophlebitis.
- Eosinophil : Cerebral or spinal cysticercosis.
- Malignant Cells: Cerebral or spinal malignancy.
Normal Constitution of Cerebrospinal fluid :
- Daily about 1500 ml of CSF is formed
- Volume : 130 - 150 ml (the whole volume of CSF is replaced several times a day)
- Colour : Colourless
- Appearance : Clear
- Pressure : 60 - 150 mm of H2O (about 8-15 mm of Hg) in Spine and 200 - 250 mm of H2O in Sitting position.
- pH : 7.35 (7.3 - 7.4)
- Specific gravity : 1.007 (1.003 to 1.008)
- Protein : 15 - 45 mg/dl
- Sugar : 40 - 80 mg/dl
- Chloride : 720 - 750 mg/dl
- Sodium : 144 154 mEq/L
- Potassium : 2.0 - 3.5 mEq/L
- Creatinine : 0.5 - 1.2 mg/dl
- Urea : 5 - 15 mg/dl
- Uric acid : 0.5 - 4.5 mg/dl
- Cholesterol : 0.2 - 0.6 mg/dl
- Cells : 0-8 lymphocytes/cumm (Neutrophils absent).
Indication for CSF Examination :
- Diagnostic :
- Absolute :
- Meningitis
- Subarachnoid Haemorrhage
- Relative :
- Neurosyphilis
- Unexplained Coma
- Guillain barre Syndrome.
- Multiple Sclerosis
- Radiological
- Myelography
- Pneumoencephalography
- Absolute :
- Therapeutic :
- To Introduce Drugs :
- Methothexate 0.25 mg/kg biweekly in leukemia.
- Gentamicin 10-20 mg in Gram Negative meningitis.
- Crystalline Penicillin 10,000 20,000units in pyogenic meningitis.
- To reduce raised intro-cranial tension in Hypertensive Encephalopathy.
- To administer spinal anesthesia.
- To Introduce Drugs :
Contra-Indication for CSF Examination :
- Raised intracranial tension because of the risk of herniation of brain through foramen magnum and damaging the vital medullary centres causing death
- Marked Spinal deformity
- Local infection
- Suspected Cord compression.
Collection of Cerebrospinal fluid :
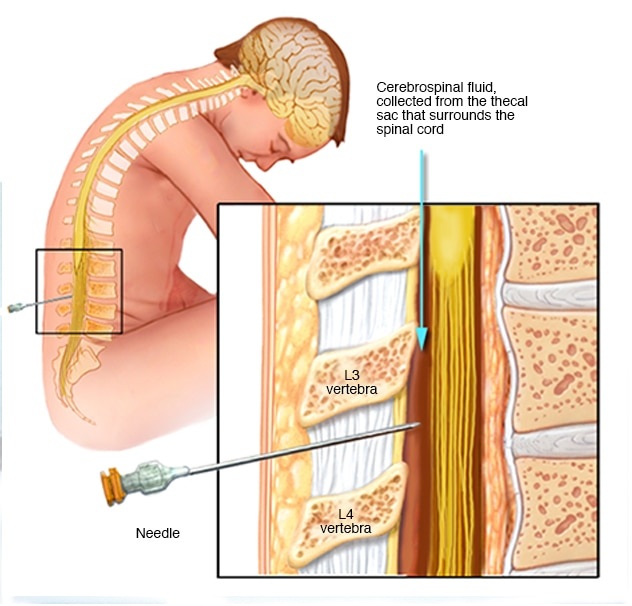
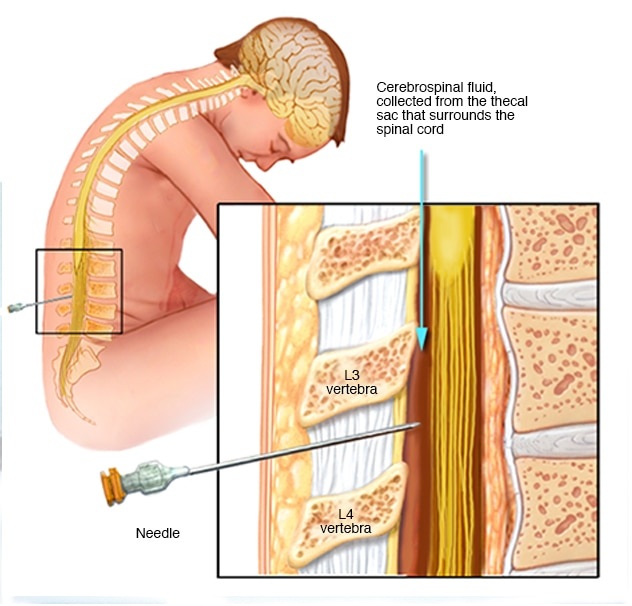
- Position : The patient is placed on his side at the edge of the bed with the knee drawn up and the head flexed. It can also be done with the patient sitting and bending forward.
- Site : In the 3rd lumber space. This space lies in the plane which joints the highest points on the iliac crest. The skin over the back from the lower thoracic vertebrae to the coccyx is sterilized with cetavlon, ether, Iodine and spirit. The part is draped.
- Local anesthesia : The skin to be punctured is infiltrated with 5 ml of 2% lignocaine. Infiltration is done upto ligamentum flava.
- Puncture : A lumber puncture needle with a stilette is introduced after 2-3 minutes into the anesthetized space, with the cutting edge of the bevel in the direction parallel to the fibers of the ligamentum flava. The needle is introduced through the resistance of supraspinous ligament. The interspious ligament is then easily negotiated. At about 4-7 cm, the firmer resistance of ligamentum flavum popping sensation as the dura is breached. The stilette is then withdrawn and the fluid is collected slowly in 4-5 sterile test tubes for biochemical, cytological and serological assay. The first few drops are collected separately and may be used for bacteriological culture.
- Seal : The needle is withdrawn and the puncture mark is sealed with a tincture benzoin seal.
- Post-procedure orders :
- Plenty of fluids are to be taken by mouth.
- Head low position, with half to one block to prevent headache.
- Salicylates, if headache.
http://medicoinfo.org/cerebrospinal-fluid-csf-significance-function-collection-patient-preparation-complication-laboratory-analysis/
| Complication for CSF Collection :Haedache : This is commonest problem. To minimize this, plenty of fluids should be taken orally, head-low position is to be given and Salicylates if required. Backache. Infection : Often causing gram-negative meningitis. Medullary herniation leading to death. Injury to the blood vessels, spinal cord or intervertebral disc. Aggravation of symptoms from which the patient is suffering root pains, paraplegia etc. |
LABORATORY INVESTIGATION OF CEREBROSPINAL FLUID
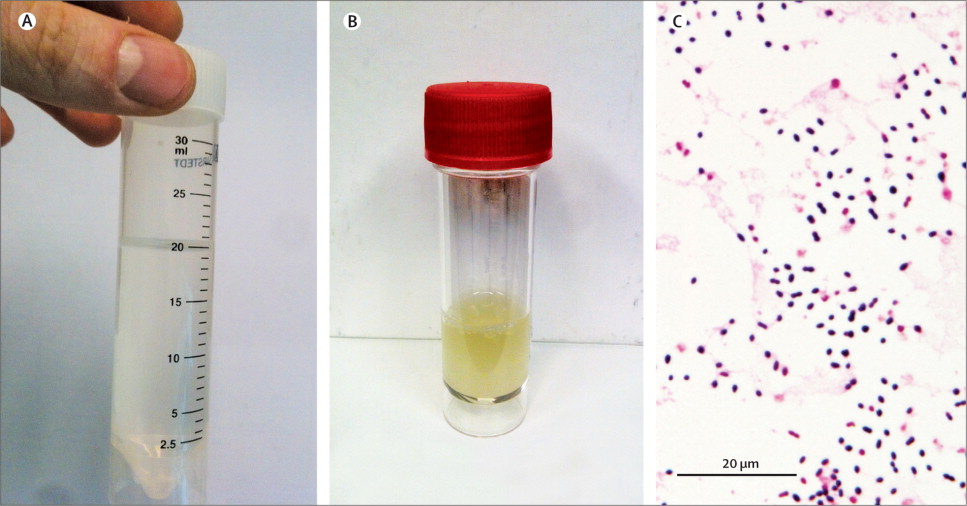
CSF must be examined immediately within one hour, after the specimen is collected. The blood cells and the offending organisms sought for diagnosis rapidly lyse on standing while the bacteria multiply with delay in analysis resulting in changes in the chemical composition (e.g. glucose). Thus, reliable reports can only be submitted if the CSF is examined fresh.
This is why a CSF specimen receives top priority ("stat") in the laboratory. The technician must also be aware of the precious nature of the specimen ( it may be impossible to collect it again), and should be very economical in handling the CSF specimen. Only a small quantity of the specimen is available and he should make a whole-hearted effort to do all the analyses requested and perform the test with extra care.
A CSF specimen should never be refrigerated, especially the portion submitted for bacterial culture. The commonly sought pathogen, Neisseria meningitidis, is killed by exposure to cold. In addition, the CSF specimen must be handled carefully to avoid biological hazard; it may contain virulent organisms that may infect the technician; a rubber pipettes to draw up the fluid.
Always discard the pipettes used for transferring CSF specimen in 5% Lysol for overnight. Discard all unused specimens in phenol solution and sterilize all glassware after soaking in disinfectant. Laboratory investigations of Cerebrospinal fluid are consist of mainly the primary examination; A) Physical Examination, B) Microscopic Examination and C) Chemical Examination.
A. Physical Examination
Physical examination ( mainly appearance and clot formation) is done with an Uncentrifuged specimen. Initial clot formation is noted before the centrifugation while one of the tubes can be left for observing 24-hour clotting, or leave the supernatant to observe clotting after processing the sediment. Leukocyte count of CSF requires a uncentrifuged whole specimen and must be done as early as possible. For chemical analysis, clear supernatant without cellular materials is desirable. The first tube (if bloody) is always discarded or used for bacterial culture while the other tubes are used for microscopic examination of the whole specimen (leukocyte count) or examination of the smear of the sediment. The sediment(more concentrated) should be used for bacterial culture.
Appearance :
Examine the appearance of CSF and record accurately as- clear, cloudy, blood-stained, or Xanthochromic. Determine the specific gravity of CSF with the help of a hand Refractometer or by the weight method. Meningitis often brings about changes in the general appearance of CSF and this can be diagnostic. Normal CSF is crystal clear and colourless. It may contain a few blood cells. When a pathologic condition is present, there may be a change in colour; Blood, pus, bacteria, and their products may be found. Pus formation due to infection leads to cloudy CSF which is most often associated with an increase in this number of pus cells or leukocytes.
Clot formation :
Normal spinal fluid does not coagulate or clot. Clot formation is due to the presence of fibrinogen which converts to fibrin to produce the clot. Fibrinogen is absent in normal CSF but increases when the blood-brain barrier is disturbed. Normal CSF does not clot and a clot formation indicates abnormality. The type of clot depends on certain diseases and is associated with increased protein concentration. A delicate, fine clot is typical of tuberculous meningitis; a large clot is associated with purulent meningitis; and a complete and spontaneous clot is found in case of spinal constriction.
http://medicoinfo.org/cerebrospinal-fluid-csf-significance-function-collection-patient-preparation-complication-laboratory-analysis/
B. MICROSCOPIC EXAMINATION
Microscopic examination of the CSF includes the Leukocyte count of the uncentrifuged whole specimen, examination of the wet mount is used for detection of Trypanosoma and Cryptococcus by using India Ink preparation. The sediment of the centrifuged specimen is taken for the study of the stained smear; Direct examination of the specimen for infectious agents & for the differential count.
Total Leukocyte Count :
Normal CSF is virtually free of cells, although as many as 5 WBC/mm3 is considered as normal and these are small mononuclear cells (lymphocytes). The presence of neutrophils and/or monocytes are the indication of abnormality. The presence of erythrocytes is also abnormal. Increased leukocyte count suggests the possibility of infective meningitis. 2% Acetic acid with 5 drops of 3% Methylene blue; This diluting fluid is most commonly used and it removes the erythrocytes and stain the leukocytes from the CSF specimen. Use the diluent only if the specimen is cloudy which indicates the possibility of increased leukocyte count.
- Gently mixed the CSF specimen.
- Dilute the specimen (1:2 dilution) only when the specimen is cloudy. A cloudy specimen may have a high leukocyte count (>500 WBC/cu.mm).
- Dilute the specimen 1:10 dilution with WBC diluting fluid or with Diluent (2% Acetic acid with 5 drops of 3% Methylene blue) in a test tube.
- Wait for 5 minutes afterwards load the counting chamber and leave the chamber for 5 minutes to allow the cells to settle.
- Count the numbers of cells present in all 16 squares under low power objective.
Differential Leukocyte Count :
The Differential Leukocyte Count provides information regarding the relative distribution of various white blood cells - lymphocytes, neutrophils and others. The basic procedure is the same as describe under haematology. Increased lymphocyte count is an indication of possible viral infection while increase neutrophils suggest bacterial infection. Preparation of a thin smear of uncentrifuged, well mixed CSF specimen on a microscopic slide for differential leukocyte count (as like haematology), if the specimen is cloudy and Total Leukocyte count of CSF is >500 WBC/cumm. If the specimen is not cloudy but Total Leukocyte count is <200 WBC/cumm then centrifuge the specimen and prepare a smear with sediment of CSF.
- Centrifuge the specimen in a centrifuge tube at 2500 rpm for 10 minutes.
- Transfer the supernatant to another tube for chemical analysis. Save the last drop of the specimen.
- Tap the sediment to mix with the last drop of fluid in the centrifuge tube.
- Prepared a smear on a clean and dry glass slide and leave to dry.
- Stain with Leishman stain or Fixed the smear with methanol & stain with methylene blue.
- Make a differential leukocyte count under 1000X magnification (oil immersion) of the microscope.
Wet mount Preparation of CSF :
Wet mount of CSF is prepare in case of suspected sleeping sickness (Trypanosomiasis) and Cryptococcosis. Trypanosomes are motile, flagellate, intercellular protozoa found in the blood at early stage of infection; their presence in CSF indicates late stage of the disease.
- Place a drop of suspended CSF sediment on a clean and dry glass slide.
- Put a coverslip on the drop.
- Examine under the high power objective (40X). Look for motile flagellates. In case of positive finding it may correlated with increased lymphocyte count, Increased globulin level and presence of mononuclear vacuolated large cells etc.
[Note : India-Ink Preparation is applied in the diagnosis of Cryptococcal infection. Sediment of Cerebrospinal fluid is used for Gram staining and Acid Fast staining.]
http://medicoinfo.org/cerebrospinal-fluid-csf-significance-function-collection-patient-preparation-complication-laboratory-analysis/
Culture and Sensitivity test of CSF :
The first tube is always used for bacterial culture while the other tubes are used for microscopic examination of the whole specimen (leukocyte count) or examination of the smear of the sediment. The sediment (more concentrated) should be used for bacterial culture. The common pathogenic bacteria responsible for meningeal problems are : Neisseria meningitidis, Haemophilus influenzae, Streptococcus pneumonia and Mycobacterium tuberculosis.
C. Chemical Examination of CSF
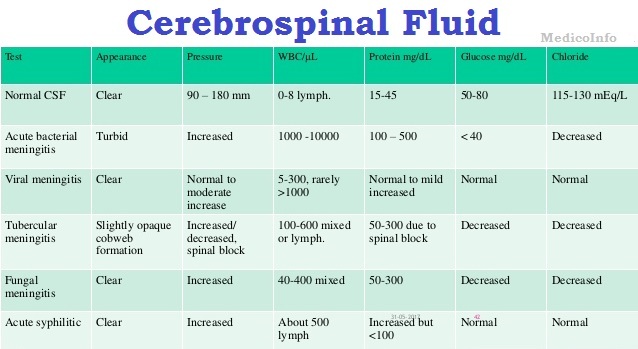
Chemical examination of Cerebrospinal fluid (particularly glucose, Total Protein and Globulin) play an important role for detect the nature of meningitis.
Glucose level in spinal fluid is about 40 - 80 mg/dl. The glucose level in spinal fluid is especially reduced in bacterial meningitis which may be due to increase number of leukocytes and pathogenic organisms and both contribute to increased glycolysis. Decreased CSF glucose level is not seen in viral meningitis, primary brain tumour or vascular accidents. It is low in metastatic tumour and insulin shock and elevated in diabetic coma. Increased CSF glucose level is seen in some pathogenic states such as brain tumour (70 - 100 mg/dl) and also in case of diabetes mellitus. Benedict quantitative test, Orthotoluidine test and GOD-POD enzymatic methods are used for determination of glucose concentration of CSF.
Total Protein concentration of Cerebrospinal fluid is about 15 - 45 mg/dl, which is below 1% of the normal serum protein level. Incase of inflammation of the meninges under toxic conditions or development of tumours, the barriers between the blood and brain become more permeable and increased amounts of protein enter the subarachnoid space and appear in the CSF.
Globulin is the protein of chief interest in the study of CSF. This is because immunoglobulins develop within the CSF in case of infection. Blood tap gives erroneous results. Pandy test and Sulphosalicylic acid turbidometry tests are convenient semiquantitative procedures for globulin and total protein respectively.


Thank you for the excellent article. Please Continue…..
This is a very good tip especially to those new to the blogosphere.
Simple but very precise information… Thanks for sharing this one. A must read article!
I believe the content material here is rattling fantastic , appreciate it for your efforts. You should keep it up forever! Best of luck.
Hey This web site truly has all of the information and facts I wanted concerning this subject and didn’t know who to ask. thanks
Nice post. I learn something more challenging on totally different blogs everyday. However, I am really impressed by your blog. Keep up posting these types of posts.
Greate pieces. Keep posting such kind of info on your page. I am really impressed by your blog. Hey there, You have done an incredible job. I’ll definitely love it and for my part recommend to my friends. I am sure they will be benefited from this website.
Hello, Your blog style is amazing, It’s truly informative. Following your articles…