Systemic Lupus Erythematosus (SLE)
Systemic Lupus Erythematosus (SLE) is an autoimmune disease characterized by acute and chronic inflammation of various tissues of the body. It’s also known to as Disseminated lupus erythematosus or LE syndrome or Libman-Sacks disease or Lupus. Autoimmune diseases are illnesses that occur when the body’s tissues are attacked by its own immune system. The immune system is a complex system within the body that is designed to fight infectious agents, such as bacteria and other foreign microbes. One of the ways that the immune system fights infections is by producing antibodies that bind to the microbes. People with lupus produce abnormal antibodies in their blood that target tissues within their own body rather than foreign infectious agents. These antibodies are referred to as autoantibodies.
Because the antibodies and accompanying cells of inflammation can affect tissues anywhere in the body, lupus has the potential to affect a variety of areas. Sometimes lupus can cause disease of the skin, heart, lungs, kidneys, joints, nervous system, and/or blood-forming (hematopoietic) system. When only the skin is involved by rash, the condition is called lupus dermatitis or cutaneous lupus erythematosus. A form of cutaneous lupus erythematosus that can be isolated to the skin, without internal disease, is called discoid lupus erythematosus. When internal organs are involved, the condition is referred to as systemic lupus erythematosus (SLE).Both discoid lupus erythematosus and systemic lupus are more common in women than men (about eight times more common). The disease can affect all ages but most commonly begins from 20-45 years of age. Statistics demonstrate that lupus is somewhat more frequent in African Americans and people of Chinese and Japanese descent. Systemic Lupus Erythematosus (SLE) has been estimated to affect about 322,000 people worldwide and 1.5 million people in the United States. The exact prevalence is difficult to determine because many of the signs and symptoms of SLE resemble those of other disorders. Diagnosis may be delayed for years, and the condition may never be diagnosed in some affected individuals. Females develop SLE about nine times more often than males. It is most common in younger women, peaking during the childbearing years; however, 20 percent of SLE cases occur in people over age 50.
For unknown reasons, in industrialized Western countries SLE has become 10 times more common over the past 50 years. The prevalence of SLE in Africa and Asia is believed to be much lower than in Western nations; however, in industrialized Western countries, people of African and Asian descent are two to four times more likely to develop SLE than are people of European descent. Researchers suggest that factors such as ethnic mixing, tobacco use in industrialized countries, and the different types of infections people acquire in different regions may contribute to these differences. For example malaria, which occurs often in tropical regions, is thought to be protective against SLE, while the Epstein-Barr virus, more common in the West, increases SLE risk.
Causes & Risk Factors of Systemic Lupus Erythematosus :
Normal variations (polymorphisms) in many genes can affect the risk of developing SLE, and in most cases multiple genetic factors are thought to be involved. In rare cases, SLE is caused by mutations in single genes. Most of the genes associated with SLE are involved in immune system function, and variations in these genes likely affect proper targeting and control of the immune response. Sex hormones and a variety of environmental factors including viral infections, diet, stress, chemical exposures, and sunlight are also thought to play a role in triggering this complex disorder. About 10 percent of SLE cases are thought to be triggered by drug exposure, and more than 80 drugs that may be involved have been identified.
In people with SLE, cells that have undergone self-destruction (apoptosis) because they are damaged or no longer needed are not cleared away properly. The relationship of this loss of function to the cause or features of SLE is unclear. Researchers suggest that these dead cells may release substances that cause the immune system to react inappropriately and attack the body’s tissues, resulting in the signs and symptoms of SLE.
The precise reason for the abnormal autoimmunity that causes lupus is not known. Inherited genes, viruses, ultraviolet light, and certain medications may all play some role. Lupus is not caused by an infectious microorganism and is not contagious from one person to another.
Genetic factors increase the tendency of developing autoimmune diseases, and autoimmune diseases such as lupus, rheumatoid arthritis, and autoimmune thyroid disorders are more common among relatives of people with lupus than the general population. Moreover, it is possible to have more than one autoimmune disease in the same individual. Therefore, “overlap” syndromes of lupus and rheumatoid arthritis, or lupus and scleroderma, etc., can occur.
Some scientists believe that the immune system in lupus is more easily stimulated by external factors like viruses or ultraviolet light. Sometimes, symptoms of lupus can be precipitated or aggravated by only a brief period of sun exposure.
It also is known that some women with systemic lupus erythematosus can experience worsening of their symptoms prior to their menstrual periods. This phenomenon, together with the female predominance of systemic lupus erythematosus, suggests that female hormones play an important role in the expression of SLE. This hormonal relationship is an active area of ongoing study by scientists.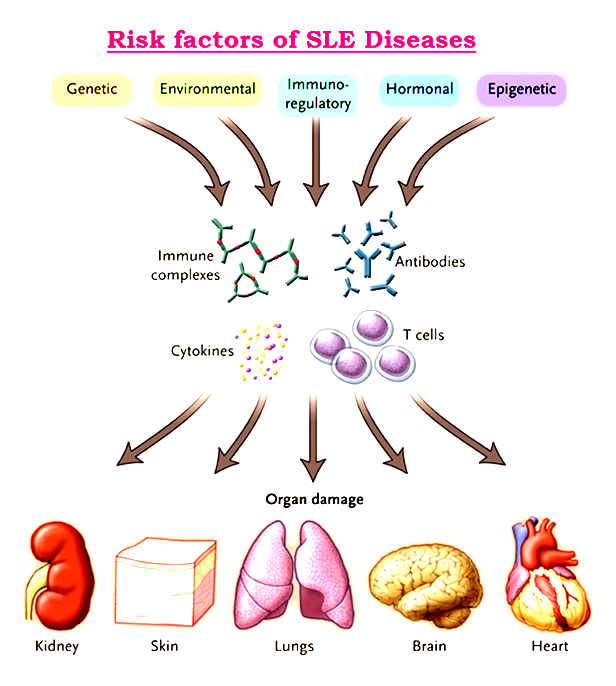 Research has demonstrated evidence that a key enzyme’s failure to dispose of dying cells may contribute the development of systemic lupus erythematosus. The enzyme, DNase1, normally eliminates what is called “garbage DNA” and other cellular debris by chopping them into tiny fragments for easier disposal. Researchers turned off the DNase1 gene in mice. The mice appeared healthy at birth, but after six to eight months, the majority of mice without DNase1 showed signs of systemic lupus erythematosus. Thus, a genetic mutation in a gene that could disrupt the body’s cellular waste disposal may be involved in the initiation of systemic lupus erythematosus.
Research has demonstrated evidence that a key enzyme’s failure to dispose of dying cells may contribute the development of systemic lupus erythematosus. The enzyme, DNase1, normally eliminates what is called “garbage DNA” and other cellular debris by chopping them into tiny fragments for easier disposal. Researchers turned off the DNase1 gene in mice. The mice appeared healthy at birth, but after six to eight months, the majority of mice without DNase1 showed signs of systemic lupus erythematosus. Thus, a genetic mutation in a gene that could disrupt the body’s cellular waste disposal may be involved in the initiation of systemic lupus erythematosus.
Dozens of medications have been reported to trigger Systemic Lupus Erythematosus (SLE). However, more than 90% of cases of “drug-induced lupus” occurs as a side effect of one of the following six drugs:
Hydralazine (Apresoline) is used for high blood pressure.
- Quinidine (Quinidine Gluconate, Quinidine Sulfate) and procainamide (Pronestyl; Procan-SR; Procanbid) are used for abnormal heart rhythms.
- Phenytoin (Dilantin) is used for epilepsy.
- Isoniazid (Nydrazid, Laniazid) is used for tuberculosis. and
- d-penicillamine (used for rheumatoid arthritis)
Sign & Symptoms of Systemic Lupus Erythematosus :
Symptoms of systemic lupus erythematosus (SLE, often referred to as simply lupus) can be quite different, because there are different types of lupus, and not all affected people show the same symptoms. It may come on suddenly or develop slowly, may be mild or severe, and may be temporary or permanent. Most people with lupus have mild disease characterized by episodes – called flares – when signs and symptoms get worse for a while, then improve or even disappear completely for a time.The signs and symptoms of lupus that you experience will depend on which body systems are affected by the disease. People with SLE can develop different combinations of symptoms and organ involvement. The most common signs and symptoms include:
- Muscle and joint pain : Patient may experience pain and stiffness, with or without swelling. This affects most people with Systemic Lupus Erythematosus. Common areas for muscle pain and swelling include the neck, thighs, shoulders, and upper arms.
- Fever : A fever higher than 100 degrees Fahrenheit affects many people with Systemic Lupus Erythematosus. The fever is often caused by inflammation or infection. Lupus medicine can help manage and prevent fever.
- Rashes : Patient may get rashes on any part of your body that is exposed to the sun, such as face, arms, and hands. One common sign of Systemic Lupus Erythematosus is a red, butterfly-shaped rash across the nose and cheeks.
- Chest pain : Systemic Lupus Erythematosus can trigger inflammation in the lining of the lungs. This causes chest pain when breathing deeply.
- Hair loss : Patchy or bald spots are common. Hair loss could also be caused by some medicines or infection.
- Sun or light sensitivity : Most people with Systemic Lupus Erythematosus are sensitive to light, a condition called photosensitivity. Exposure to light can cause rashes, fever, fatigue, or joint pain in some people with lupus.
- Kidney problems : Half of people with lupus also have kidney problems, called lupus nephritis. Symptoms include weight gain, swollen ankles, high blood pressure, and decreased kidney function.
- Mouth sores : Also called ulcers, these sores usually appear on the roof of the mouth, but can also appear in the gums, inside the cheeks, and on the lips. They may be painless, or you may have soreness or dry mouth.

- Prolonged or extreme fatigue : Patient may feel tired or exhausted even when you get enough sleep. Fatigue can also be a warning sign of a lupus flare.
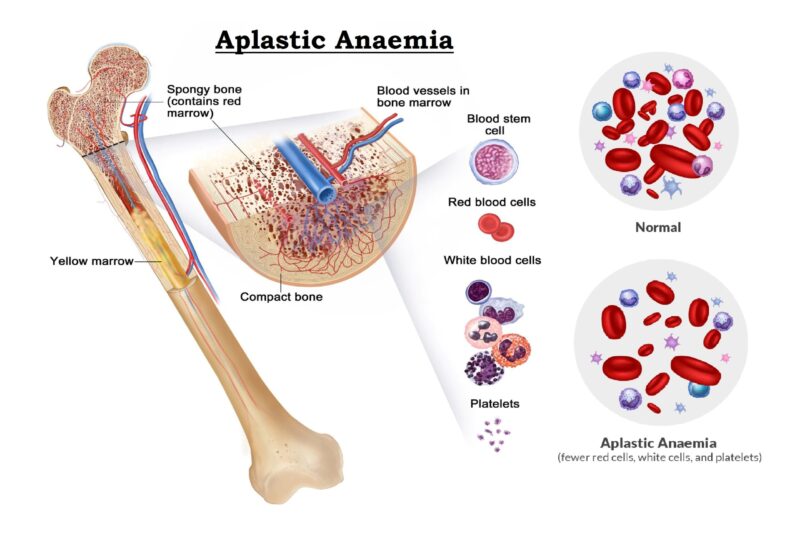
- Anemia : Fatigue could be a sign of anemia, a condition that happens when body does not have red blood cells to carry oxygen throughout body.
- Memory problems : Some people with lupus report problems with forgetfulness or confusion.
- Blood clotting : Patient may have a higher risk of blood clotting. This can cause blood clots in the legs or lungs, stroke, heart attack, or repeated miscarriages.
- Eye disease : Patient may get dry eyes, eye inflammation, and eyelid rashes.
Complication of Systemic Lupus Erythematosus :
Complications of organ involvement can lead to further symptoms that depend on the organ affected and severity of the disease.
- SLE-associated skin manifestations can sometimes lead to scarring. In discoid lupus, only the skin is typically involved. The skin rash in discoid lupus often is found on the face and scalp. It usually is red and may have raised borders. Discoid lupus rashes are usually painless and do not itch, but scarring can cause permanent hair loss (alopecia). Over time, 5%-10% of those with discoid lupus may develop SLE.
Over half of the people with SLE develop a characteristic red, flat facial rash over the bridge of their nose. Because of its shape, it is frequently referred to as the “butterfly rash” of SLE. The rash is painless and does not itch. The facial rash, along with inflammation in other organs, can be precipitated or worsened by exposure to sunlight, a condition called photosensitivity. This photosensitivity can be accompanied by worsening of inflammation throughout the body, called a “flare” of the disease. Typically, with treatment, this rash can heal without permanent scarring. - Most SLE patients will develop arthritis during the course of their illness. Arthritis from SLE commonly involves swelling, pain, stiffness, and even deformity of the small joints of the hands, wrists, and feet. Sometimes, the arthritis of SLE can mimic that of rheumatoid arthritis (another autoimmune disease).
- More serious organ involvement with inflammation occurs in the brain, liver, and kidneys. White blood cells can be decreased in SLE (referred to as leukopenia or leucopenia). Also, low blood-clotting factors called platelets (thrombocytopenia) can be caused by lupus. Leukopenia can increase the risk of infection, and thrombocytopenia can increase the risk of bleeding. Low red blood cell counts (hemolytic anemia) can occur. Inflammation of muscles (myositis) can cause muscle pain and weakness. This can lead to elevations of muscle enzyme levels in the blood.
- Inflammation of blood vessels (vasculitis) that supply oxygen to tissues can cause isolated injury to a nerve, the skin, or an internal organ. The blood vessels are composed of arteries that pass oxygen-rich blood to the tissues of the body and veins that return oxygen-depleted blood from the tissues to the lungs. Vasculitis is characterized by inflammation with damage to the walls of various blood vessels. The damage blocks the circulation of blood through the vessels and can cause injury to the tissues that are supplied with oxygen by these vessels.Inflammation of the lining of the lungs (pleuritis) with pain aggravated by deep breathing (pleurisy) and of the heart (pericarditis) can cause sharp chest pain. The chest pain is aggravated by coughing, deep breathing, and certain changes in body position. The heart muscle itself rarely can become inflamed (carditis). It has also been shown that young women with SLE have a significantly increased risk of heart attacks due to coronary artery disease.
- Kidney inflammation in SLE (lupus nephritis) can cause leakage of protein into the urine, fluid retention, high blood pressure, and even kidney failure. This can lead to further fatigue and swelling (edema) of the legs and feet. With kidney failure, machines are needed to cleanse the blood of accumulated waste products in a process called dialysis.
- Involvement of the brain can cause personality changes, thought disorders (psychosis), seizures, and even coma. Lupus of the nervous system (neurologic lupus) can lead to damage to nerves cause numbness, tingling, and weakness of the involved body parts or extremities. Brain involvement is referred to as lupus cerebritis.
- Many people with SLE experience hair loss (alopecia). Often, this occurs simultaneously with an increase in the activity of their disease. The hair loss can be patchy or diffuse and appear to be more like hair thinning.
- Some people with SLE have Raynaud’s phenomenon. Raynaud’s phenomenon causes the blood vessels of the hands and feet to spasm, especially upon exposure to cold. The blood supply to the fingers and/or toes then becomes compromised, causing blanching, whitish and/or bluish discoloration, and pain and numbness in the exposed fingers and toes.
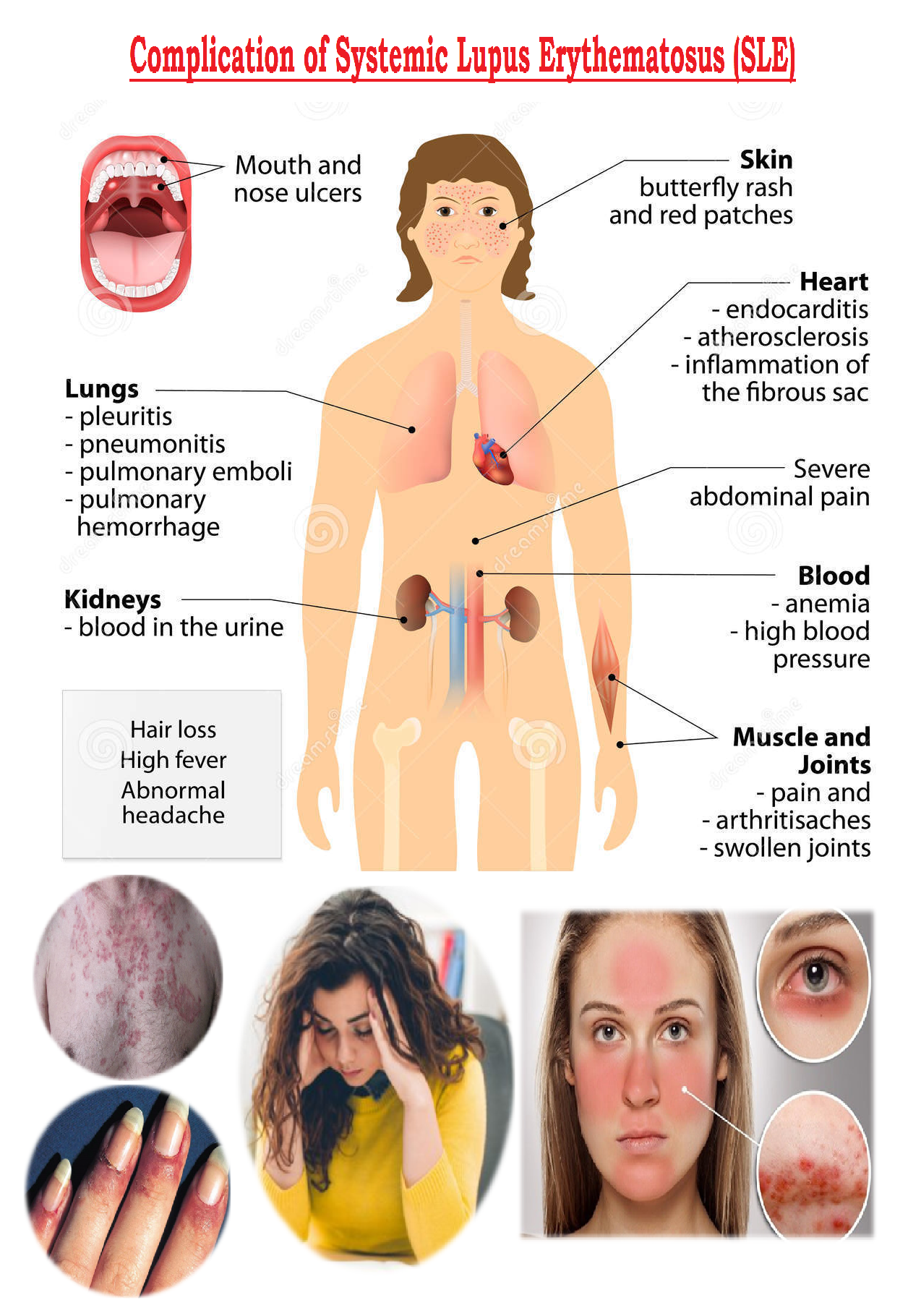
- Other diseases and conditions that can accompany lupus include fibromyalgia, Coronary Heart Disease (CHD), nonbacterial valvular heart disease, pancreatitis, esophagus disease with difficulty swallowing (dysphagia), swollen lymph nodes (lymphadenopathy), liver disease (lupoid hepatitis), infections, and a tendency to spontaneous blood clotting and thrombosis.
Diagnosis of Systemic Lupus Erythematosus :
Since SLE patients can have a wide variety of symptoms and different combinations of organ involvement, no single blood test establishes the diagnosis of systemic lupus. To help doctors improve the accuracy of the diagnosis of SLE, 11 criteria were established by the American Rheumatism Association. These 11 criteria are closely related to the symptoms discussed above. Some people suspected of having SLE may never develop enough criteria for a definite diagnosis. Other people accumulate enough criteria only after months or years of observation. When a person has four or more of these criteria, the diagnosis of SLE is strongly suggested. Nevertheless, the diagnosis of SLE may be made in some settings in people with only a few of these classical criteria, and treatment may sometimes be instituted at this stage. Of these people with minimal criteria, some may later develop other criteria, but many never do.The following are 11 criteria used for diagnosing systemic lupus erythematosus:
-
- Malar rash (over the cheeks of the face).
- Discoid skin rash (patchy redness with hyperpigmentation and hypopigmentation that can cause scarring).
- Photosensitivity [skin rash in reaction to sunlight (ultraviolet light) exposure].
- Mucous membrane ulcers (spontaneous sores or ulcers of the lining of the mouth, nose, or throat).
- Arthritis (two or more swollen, tender joints of the extremities).
- Pleuritis or pericarditis (inflammation of the lining tissue around the heart or lungs, usually associated with chest pain upon breathing or changes of body position).
- Kidney abnormalities (abnormal amounts of urine protein or casts detectable with a standard urinalysis). Ultimately, in patients with kidney disease from systemic lupus erythematosus (lupus nephritis), a kidney biopsy may be necessary to both define the cause of the kidney disease as being lupus-related as well as to determine the stage of the kidney disease in order to optimally guide treatments.
- Brain irritation (manifested by seizures [convulsions] and/or psychosis, referred to as “lupus cerebritis”)
- Blood Cell Count abnormalities: low white blood count (WBC) or red blood count (RBC), or platelet count on routine complete blood count testing; leukopenia, anemia, and thrombocytopenia, respectively. Each of these are detectable with standard complete blood count testing (CBC).
- Immunologic disorder (abnormal immune tests include anti-double-stranded DNA (anti-dsDNA) or anti-Sm [anti-Smith] antibodies, falsely positive blood test for syphilis, anticardiolipin antibodies, lupus anticoagulant, or positive LE prep test)
- Antinuclear antibody (positive ANA antibody testing [antinuclear antibodies in the blood])
In addition to the 11 criteria, other tests can be helpful in evaluating people with SLE to determine the severity of organ involvement. These include routine testing of the blood to detect inflammation (for example, the Erythrocyte Sedimentation Rate or ESR, and the C-reactive protein, or CRP), blood-chemistry testing, direct analysis of internal body fluids, and tissue biopsies. Abnormalities in body fluids (joint or cerebrospinal fluid) and tissue samples (kidney biopsy, skin biopsy, and nerve biopsy) can further support the diagnosis of SLE. The appropriate testing procedures are selected for the patient individually by the doctor.
The combination of blood and urine tests, signs and symptoms and physical examination findings leads to the diagnosis. Common test are as follows :
A. Laboratory tests (Blood and urine tests) :
-
- Complete blood count : This test measures the number of red blood cells, white blood cells and platelets as well as the amount of hemoglobin. Results may indicate patient have anemia, which commonly occurs in Systemic Lupus Erythematosus. A low white blood cell or platelet count may occur in Systemic Lupus Erythematosus as well.
- Erythrocyte Sedimentation Rate (ESR) : This blood test determines the rate at which red blood cells settle to the bottom of a tube in first hour. A faster than normal rate may indicate a systemic disease, such as Systemic Lupus Erythematosus. The Erythrocyte Sedimentation Rate isn’t specific for any one disease. It may be elevated if the patient have Systemic Lupus Erythematosus, an infection, another inflammatory condition or cancer.
- Kidney and liver assessment : Blood tests can assess how well kidneys and liver are functioning. Systemic Lupus Erythematosus can affect these organs.
- Urinalysis : An examination of a sample of urine may show an increased protein level or red blood cells in the urine, which may occur if Systemic Lupus Erythematosus has affected patient kidneys.
- Antinuclear antibody (ANA) test : A positive test for the presence of these antibodies — produced by immune system — indicates a stimulated immune system. While most people with lupus have a positive ANA test, most people with a positive ANA do not have lupus. If you test positive for ANA, doctor may advise more-specific antibody testing.
If doctor suspects that lupus is affecting lungs or heart, he or she may suggest:
-
- Chest X-ray : An image of chest may reveal abnormal shadows that suggest fluid or inflammation in the lungs.
- Echocardiogram : This test uses sound waves to produce real-time images of beating heart. It can check for problems with valves and other portions of the heart.
C. Biopsy
Lupus can harm kidneys in many different ways, and treatments can vary, depending on the type of damage that occurs. In some cases, it’s necessary to test a small sample of kidney tissue to determine what the best treatment might be. The sample can be obtained with a needle or through a small incision. Skin biopsy is sometimes performed to confirm a diagnosis of lupus affecting the skin.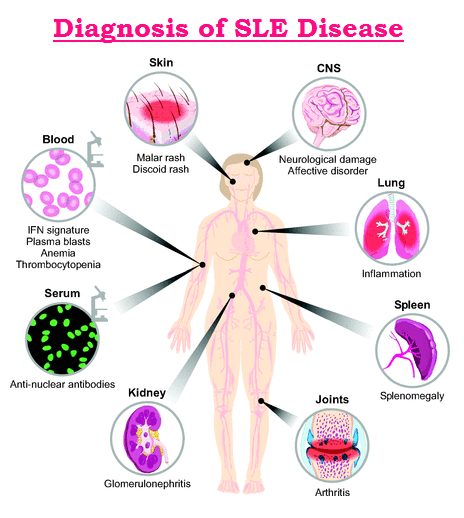
Treatment of Systemic Lupus Erythematosus :
There is no permanent cure for SLE. The goal of treatment is to relieve symptoms and protect organs by decreasing inflammation and/or the level of autoimmune activity in the body. The precise treatment is decided on an individual basis. Many people with mild symptoms may need no treatment or only intermittent courses of anti-inflammatory medications. Those with more serious illness involving damage to internal organ(s) may require high doses of corticosteroids in combination with other medications that suppress the body’s immune system.People with SLE need more rest during periods of active disease. Researchers have reported that poor sleep quality was a significant factor in developing fatigue in people with SLE. These reports emphasize the importance for people and physicians to address sleep quality and the effect of underlying depression, lack of exercise, and self-care coping strategies on overall health. During these periods, carefully prescribed exercise is still important to maintain muscle tone and range of motion in the joints. To protect from sun sensitivity, sunscreens, sun avoidance, and sun protection clothing are used. Certain types of lupus rash can respond to topical cortisone medications.
Treatment for lupus depends on the signs and symptoms of patients. Determining whether signs and symptoms should be treated and what medications to use requires a careful discussion of the benefits and risks with doctor. As signs and symptoms flare and subside, patient and doctor may find that patient will need to change medications or dosages. The medications most commonly used to control lupus include:
-
- Nonsteroidal anti-inflammatory drugs (NSAIDs) : Over-the-counter NSAIDs, such as naproxen sodium (Aleve) and ibuprofen (Advil, Motrin IB, others), may be used to treat pain, swelling and fever associated with SLE. Stronger NSAIDs are available by prescription. Side effects of NSAIDs include stomach bleeding, kidney problems and an increased risk of heart problems. . The most common side effects are stomach upset, abdominal pain, ulcers, and even ulcer bleeding. NSAIDs are usually taken with food to reduce side effects.
- Antimalarial drugs : Hydroxychloroquine (Plaquenil) is an antimalarial medication found to be particularly effective for SLE patients with fatigue, skin involvement, and joint disease. Consistently taking Plaquenil can prevent flare-ups of lupus. Side effects are uncommon but include diarrhea, upset stomach, and eye-pigment changes. Eye-pigment changes are rare but require monitoring by an ophthalmologist (eye specialist) during treatment with Plaquenil. Plaquenil significantly decreased the frequency of abnormal blood clots in people with systemic lupus.
Moreover, the effect seemed independent of immune suppression, implying that Plaquenil can directly act to prevent the blood clots. This fascinating study highlights an important reason for people and doctors to consider Plaquenil for long-term use, especially for those SLE people who are at some risk for blood clots in veins and arteries, such as those with phospholipid antibodies (cardiolipin antibodies, lupus anticoagulant, and false-positive venereal disease research laboratory test). This means not only that Plaquenil reduces the chance for re-flares of SLE, but it can also be beneficial in thinning the blood to prevent abnormal excessive blood clotting. Plaquenil is commonly used in combination with other treatments for lupus.
For resistant skin disease, other antimalarial drugs, such as chloroquine (Aralen) or quinacrine, are considered and can be used in combination with hydroxychloroquine. Alternative medications for skin disease include dapsone and retinoic acid (Retin-A). Retin-A is often effective for an uncommon wart-like form of lupus skin disease. For more severe skin disease, immunosuppressive medications are considered as described below. Side effects can include stomach upset and, very rarely, damage to the retina of the eye. - Corticosteroids : Corticosteroids are more potent than NSAIDs in reducing inflammation and restoring function when the disease is active. Corticosteroids are particularly helpful when internal organs are affected. Corticosteroids can be given by mouth, injected directly into the joints and other tissues, or administered intravenously. Unfortunately, corticosteroids have serious side effects when given in high doses over prolonged periods, and the doctor will try to monitor the activity of the disease in order to use the lowest doses that are safe. Side effects of corticosteroids include weight gain, thinning of the bones and skin, infection, diabetes, facial puffiness, cataracts, and death (necrosis) of the tissues in large joints. The risk of side effects increases with higher doses and longer term therapy.
- Immunosuppressants : Drugs that suppress the immune system may be helpful in serious cases of lupus. Examples include azathioprine (Imuran, Azasan), mycophenolate (CellCept), leflunomide (Arava) and methotrexate (Trexall). Potential side effects may include an increased risk of infection, liver damage, decreased fertility and an increased risk of cancer. All immunosuppressive medications can seriously depress blood-cell counts and increase risks of infection and bleeding. Immunosuppressive medications may not be taken during pregnancy or conception because of risk to the fetus. Other side effects are specific for each drug. For examples, methotrexate can cause liver toxicity, while cyclosporine can impair kidney function. In recent years, mycophenolate mofetil (CellCept) has been used as an effective medication for lupus, particularly when it is associated with kidney disease. CellCept has been helpful in reversing active lupus kidney disease (lupus renal disease) and in maintaining remission after it is established. Its lower side-effect profile has advantage over traditional immune-suppression medications.
- Plasmapheresis : In lupus patients with serious brain (lupus cerebritis) or kidney disease (lupus nephritis), plasmapheresis is sometimes used to remove antibodies and other immune substances from the blood to suppress immunity. Plasmapheresis is a process of removing blood and passing the blood through a filtering machine, then returning the blood to the body with its antibodies removed. Rarely, people with SLE can develop seriously low platelet levels, thereby increasing the risk of excessive and spontaneous bleeding. Since the spleen is believed to be the major site of platelet destruction, surgical removal of the spleen is sometimes performed to improve platelet levels. Other treatments have included plasmapheresis and the use of male hormones.
Plasmapheresis has also been used to remove certain harmful proteins (cryoglobulins) that can lead to vasculitis. End-stage kidney damage from SLE requires dialysis and/or a kidney transplant. - Antibody therapy : Research is indicating benefits of rituximab (Rituxan) in treating lupus. Rituximab is an intravenously infused antibody that suppresses a particular white blood cell, the B cell, by decreasing their number in the circulation. B cells have been found to play a central role in lupus activity, and when they are suppressed, the disease tends toward remission. This may particularly helpful for people with kidney disease.
- Biologics : Another new B-cell-suppressing treatment is belimumab (Benlysta). Belimumab blocks the stimulation of the B cells (a B-lymphocyte stimulator or BLyS-specific inhibitor) and is approved for the treatment of adults with active autoantibody-positive systemic lupus erythematosus who are receiving standard therapy. It is important to note that the efficacy of belimumab has not been evaluated in patients with severe active lupus nephritis or severe active central nervous system lupus. Belimumab has not been studied in combination with other biologic therapies or intravenous cyclophosphamide.
Prevention of Systemic Lupus Erythematosus : :
SLE is undoubtedly a potentially serious illness with involvement of numerous organ systems. However, it is important to recognize that most people with SLE lead full, active, and healthy lives. Periodic increases in disease activity (flares) can usually be managed by varying medications. Since ultraviolet light can precipitate and worsen flares, people with systemic lupus should avoid sun exposure. Sunscreens and clothing covering the extremities can be helpful. Abruptly stopping medications, especially corticosteroids, can also cause flares and should be avoided. People with SLE are at increased risk of infections as SLE-related complications, especially if they are taking corticosteroids or immunosuppressive medications. Things can do at home to help control symptoms of lupus include:
-
- Medication that treats inflammation and delays disease progression.
- Medicinal infusions or injections.
- Treatment of lupus-related health conditions (high cholesterol, high blood pressure, or infection).
- Regular exercise.
- Eating a healthy diet.
- Avoiding tobacco products.
- Using sun protection.
- Getting plenty of vitamin D and omega-3 fatty acids.
Therefore, any unexpected fever should be reported to medical professionals and evaluated.




Hello ,It’s always interesting to read content from other authors and practice something from their sites. Thank You
Thanks to my father who told me concerning this weblog, this weblog is actually amazing. gracious
I just signed up to your blog feed after reading this post! very informative, can you write more regarding this in future articles?