Microscopic Examination of Urine
The Microscopic examination of urine is a valuable diagnostic tool for the detection and evaluation of renal and urinary tract disorders and other systemic diseases. For microscopic examination, a clean voided early morning specimen and also two hours after the principle meal are suitable. Early morning urine specimen is usually preferred because not only is it most concentrated but also it has a low PH (Normally, urine is slightly acidic PH-6.0), which preserved the formed elements (erythrocytes, leukocytes, epithelial cell, cast, crystal etc.) present in the urine. For screening purpose, 300 ml capacity container is used for collection of urine specimen.
 The microscopic elements present in the urine (in suspension) are collected in the form of deposit by centrifugation. A small drop of the sediment is examined by making a cover-slip preparation under microscope.
The microscopic elements present in the urine (in suspension) are collected in the form of deposit by centrifugation. A small drop of the sediment is examined by making a cover-slip preparation under microscope.
REQUIREMENTS :
- Centrifuge tube (15-ml) with test tube rack.
- Glass slide.
- Cover-slips.
- Pasteur pipettes.
- Microscope with 10X &40X objectives.
- Centrifuge machine.
- Marker pencil.
SPECIMEN :
Freshly voided, mid-stream, morning urine specimen.
Random mid-stream specimen of urine is satisfactory for screening purpose. For better morphology, it is preferable to collect a two hours voided urine specimen, after the first morning voided has been discarded.
Urine must be examined while fresh, since cells and casts begin to lyses within 1 – 3 hours. If it can’t be examined within an hour of voiding, it should be refrigerated at 4ºC. Before and after transportation of urine, a preservative should be added with the specimen.
PROCEDURE :
- Mixed the urine and poured into a clean and dry centrifuge tube until it is ¾ full (about 8-10ml).
- Centrifuged with another balanced tube for 5 minutes at 2,500 r.p.m..
- Poured off the supernatant quickly and completely into another test tube (for Chemical examination).
- Re-suspended the deposit by shaking the centrifuge tube.
- Placed one drop of the deposit on a clean and dry glass slide.
- Covered it with a cover-slip and marked it with the identification number by using a marker pencil.
- Observed the slide first under low power (10X) objective in subdued light and afterward observed under high power (40X) objective in the microscope and note the contents of various fields and give the result as per h.p.f.(high power field).
FORMED ELEMENTS FOUND IN URINE SPECIMEN :
The following formed elements are mainly found in urine :-
- Pus cells.
- Epithelial cells.
- Erythrocytes.
- Casts.
- Crystals.
- Parasites.
- Spermatozoa.
- Yeast cells.
- Bacteria. and
- Artifacts.
PUS CELLS (WBC) :
The pus cells can enter in the urine anywhere from the glomerulus to the urethra. Normal urine contain 2-3 pus cells per high power field (h.p.f.). they are mostly Neutrophil and approximately 10-12µ (micron) in diameter found in fresh voided urine. Nuclear details may be lost with onset of cellular degeneration. Pus cell are rapidly lyses by hypotonic or alkaline urine. About 50% of pus cells are lyses following 2-3 hours of standing of urine at room temperature.
An increased number (>10 cells/h.p.f.) of white cells in the urine is called pyuria. Increased number of pus cells is indicate some infection in urinary tract [in the bladder (cystitis), in the kidney (pyelonephritis)] or in female, contamination with vaginal secretions.
Pyuria can also be detected by “Leukocyte esterase reagent dipstick test” with a sensitivity of about 90% and specificity of about 80%. The strip test is valuable in pyuria of hypotonic urine where the neutrophils swell and exhibit Brownium movement. Because of the refractivity of these moving granules, such cells are called glitter cells.
PYURIA :
An increase number of leukocytes (>10 cells/h.p.f.) in the urine specimen is called pyuria. The causes of pyuria are as follows :-
- Renal :
- Infective :
- Pyelonephritis.
- Pyonephrosis.
- Renal tuberculosis.
- Non-infective :
- Hypersensitivity.
- Nephritis.
- Analgestic nephropathy.
- Lead poisoning.
- Radiation nephritis.
- Infective :
- Lower urinary tract :
- Cystitis : Infective, Radiation, Cytotoxic drugs.
- Urethritis.
- Adnexa : Perinephric abscess, Gynecological infections
EPITHELIAL CELLS :
Epithelial cell may originate from any site in the genitor-urinary tract from the proximal convoluted tube to the urethra or from vagina. Presence of a few Squamous cells (from urethra) is consider to be normal but increased shedding may indicate renal degeneration. If the urine sediment shows the presence of transitional epithelial cells (from bladder) and renal tubular cells (from pelvis), they are clinically important and should be reported. Normally few cells (3 to 5) per h.p.f. from these sites can be found in the urine due to sloughing off old cells.
Three main types of epithelial cell may be recognized:
- Tubular Epithelial cells : These are slightly larger then leukocytes and contain large round nucleus. They may be cuboidal, flat or columnar.
- Transitional Epithelial cells : These are two or four times as larger as leukocytes. They may be pear shaped or round. Occasionally these cells may contain two nuclei.
- Squamous Epithelial cells : These are large, flat and irregularly shaped. They contain abundant cytoplasm and small central nuclei.
ERYTHROCYTES :
The red blood cells (erythrocytes) present in the urine is called haematuria. Normally RBC are not found in urine. If RBCs are already lysed and the hemoglobin is released in to the urine ,the condition is called haemoglobinuria. Haemoglobinuria may result from haemolytic anaemia, incompatible blood transfusion or paroxysmal nocturnal haemoglobinuria (PNH) while haematuria may indicate bleeding in the urinary tract.
In fresh urine these cells have a normal pale or yellow appearance. They appear smooth, biconcave disks about 7µ in diameter and 2µm thick. They do not contain nuclei. In dilute (or hypotonic solution) urine, the red cells swell-up and lyses. Lysed cells appear as colourless circles (Ghost cell). In hypertonic urine the red cells are crenate.
HAEMATURIA :
The red blood cells (erythrocytes) present in the urine is called haematuria.
- Renal disease :
- Glomerulonephritis.
- Lupus nephritis.
- Interstitial nephritis associated with drug reaction.
- Papilloma.
- Tuberculosis, acute infection.
- Infarction.
- Renal vein thrombosis.
- Hydronephrosis.
- Polycentric kidney, trauma.
- Malignant nephroclerosis and occasionally acute tubular necrosis.
- Lower urinary tract disease :
- Acute and chronic infection.
- Bladder tumour.
- Calculus.
- Stricture.
- Extra-renal disease :
- Acute appendicitis.
- Salpingitis.
- Diverticulitis.
- Tumours of the colon, rectum and pelvis.
Chyluria.
CAST :
Casts are not found in normal urine except a few hyaline ones. Their presence indicates renal disorder and is often associated with proteinuria. Identification of various types of casts help in assessed the severity of the renal disorders. Urinary cast are found in the lumen of the tubules of the kidney. The renal tubules secrete a muco-protein called Tamm-horsfall protein, which is bellied to form the basic matrix of the cast. Cast can form as the result of---
- Precipitation of gelatin of Tamm-horsfall muco-protein.
- Clumping of cells on other material with in protein matrix.
- The adherence of cells or cellular material to the matrix.
- Coagulation of material within the lumen.
- Cast formation takes place in the distal and collecting tubules (since the formation of casts required acidic conditions and high solute concentration).
- Casts dissolve in alkaline urine.
- Casts have nearly parallel sides and rounded or blunted end.
- They may be concentrated, straight or curved.
Classification of the casts is based on their microscopic appearances in the urinary deposit.
- Hyaline cast : They are colourless, homogeneous, transparent or translucent with rounded ends structure consisting of coagulated protein material. Although a few may be found transiently in normal urine (exercise, old age and benign hypertension etc.). Increased numbers are seen in renal diseases (mildest).
- Granular cast : The granular casts containing large granules embedded in coagulated proteins. The casts are present due to the degeneration of epithelial cells or leukocytes or cellular casts or due to direct aggregation of serum proteins in Tamm-Horsfall muco-protein matrix. Granular casts appear with glomerular and tubular diseases that are chronic Glomerulonephritis, chronic pyelonephritis, long-standing benign nephrosclerosis and chronic lead poisoning. These are not found in normal urine specimen.
- Red cell cast : The red cell cast may contain only a few RBCs in protein matrix or there may be many cells packed closed together with no visible matrix. Presence of red cell cast in urine is always pathogenic. They are usually diagnostic of glomerular disease being found in acute Glomerulonephritis, subacute endocarditis and also in sever pyelonephritis and in renal infection.
- White cell cast : The majority of white cells that appear in the white cell cast are polymorphonuclear neutrophils. The cells may be few or many, tightly packed together. These casts may be present in renal infection and in noninfectious inflammation. They can be seen in acute pyelonephritis and in glomerular disease.
- Epithelial cast : The epithelial cells may be arranged haphazardly and vary in size and shape. These casts are rarely seen in urine. Presence of these casts indicate tubular degeneration and necrosis. It may be due to nephrotoxic agents or virus. These casts can also be present in sever chronic renal diseases.
- Fatty (Colloid) cast : Fatty casts are formed by incorporated free fat droplets or oval fat bodies. These are seen when there is fatty degeneration of the tubular epithelium. These are frequently seen in nephritic syndrome, chronic Glomerulonephritis and toxic renal poisoning.
- Waxy cast : Waxy casts have very high refractive index. These are yellow grey or colourless and have a homogenous appearance. These casts are formed after degeneration of granular cast. They are mostly found in chronic renal failure. When the waxy cast are un-usually broad, they are termed as renal failure casts.
- Cylindroids : These resemble cast but have one end which tapers out like a strand of mucous. These are frequently hyaline in nature. The exact site and mechanism of their formation are not known.
- Oval fat bodies & Fat droplets : Oval fat bodies are renal tubular cells containing highly refractile fat droplets. These may be macrophages or polymorphonuclear leukocytes (neutrophils), which have ingested lipids or have undergone fatty degeneration.
Yeast Cells :
Yeast cells are smooth, colourless and usually ovoid cells. These can vary in size and have double refractile walls. They often show budding. Unlike RBCs, they are insoluble in acid and alkaline. They also will not stain with eosin. These are mainly found in female urine due to skin and genital contamination. Yeast cells may be found in Urinary Tract Infection (UTI) patient (mainly in diabetes mellitus disease).
Spermatozoa :
Spermatozoa have oval bodies and long, thin and delicate tails. They may be present in urine of man after epileptic convulsion, nocturnal emission and in diseases of genital organ. After coitus they may be present in the urine of both the sexes.
Bacteria :
Freshly voided normal urine is generally free from bacteria. Contamination may occur from bacteria present in the urethra, vagina or other external source. Presence of large number of bacteria with many pus cells indicates Urinary Tract Infection (UTI).
Parasites :
Following parasites are some time found in urine (Normally not found). These are as follows---
- Trichomonas Vaginalis (Trophozoite) : These are more often motile protozoa with visible exastyle, about 20-25µm in diameter and flagellated.
- Schistosoma Hematobium (ovum).
- Enterobius Vermicularis (ova).
- Microfilaria : In Chyluria, the centrifuge deposit may contain microfilaria
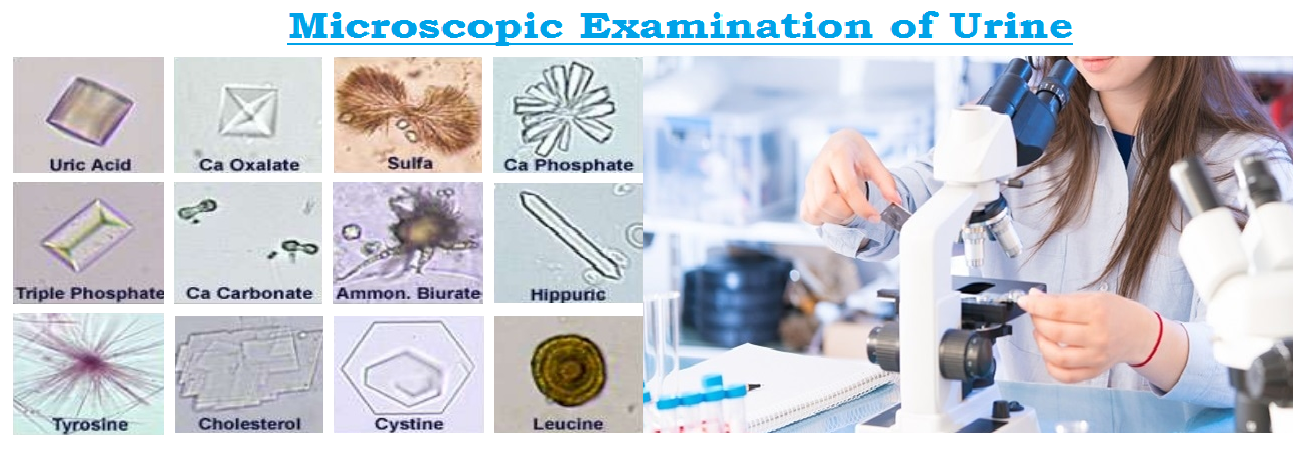
CRYSTALS :
Many of the crystals that are found in the urine have little clinical significance although they may be found in calculus formation, metabolic disorders and in the regulation of medication.
CRYSTALS FOUND IN ACIDIC URINE :
- Uric acid crystals :
- These can occur in most characteristic diamond, rhombic, rosette form, cubical or rose shaped.
- They are 30-150µm in size.
- They are usually stained with urinary pigments as yellow or red brown.
- These can soluble in sodium hydroxide and insoluble in hydrochloric acid.
- Presence of uric acid crystal can be a normal occurrence.
- Pathological condition : gout, chronic nephritis, acute febrile conditions.
- Calcium oxalate crystals :
- These are colourless and octahedral or envelop shaped, 10-20 µm in size.
- They also appear as oval, spheres or bi-concave disks. Which have a dumb-bell shape (when viewed from the side).
- These crystals are frequently found in acid and neutral urine.
- Occasionally they are also found in alkaline urine.
- They ate soluble in hydrochloric acid and insoluble in acetic acid.
- Calcium oxalate crystals can be present in urine after the ingestion of tomatoes, spinach, garlic, oranges, asparagus and vitamine-C.
- Pathological conditions : Increased number of Calcium oxalate crystals in fresh voided urine suggest the possibility of oxalate calculi, diabetes mellitus, liver disorder and chronic liver diseases etc.
- Amorphous urate crystals :
- Amorphous urate crystals are urates salt of sodium, potassium, magnesium and calcium.
- Usual form is non crystalline and/or amorphous and appear as yellow-red granules.
- They are soluble in alkaline urine at 60ºC. They have no clinical significance.
- Sodium urates crystals :
- Calcium sulfate crystals :
- They have long, thin and colourless needles or prisms.
- These are soluble in acetic acid.
- They are rarely seen in urine and they have no clinical significances.
- Hippuric acid crystals :
- These crystals are in the form of elongated prisms or plates.
- The colour may be yellow brown or colourless.
- They are soluble in water and they have no clinical significances.
- Cystine crystals :
- Cystine crystals are colourless, refractile, hexagonal plates with equal and unequal sides.
- They are 30-60 µm in size.
- They are found in patients with congenital cystinosis or congenital, cystinuria. They cab form calculi.
- Tyrosine crystal :
- These crystal are fine, refractile needles occurring in clusters or sheaves.
- They are soluble in ammonium hydroxide.
- They are found in patients with sever liver disease and tyrosinisis.
- Leucine crystals :
- Leucine crystals are oily, highly refractile spheroids with radial and concentric striations.
- They have yellow or brown colour.
- Leucine crystals are soluble in hot alcohol and acetic acid.
- They are found in patients with sever hepatitis, acute yellow atrophy and maple syrup urine disease.
- Cholesterol crystals :
- Cholesterol crystals are large, flat and transparent plates with notched corners.
- They are 50-100 µm in size and soluble in ether, chloroform and hot alcohol.
- They are found in patients with nephritic syndrome, nephritis, Chyluria and excessive tissue breakdown.
- Sulfa crystal :
- Most of the sulfa drugs precipitate out as sheaves of needles.
- They may be clear or brown in colour and usually appear with eccentric binding.
- They are soluble in acetone.



Hi, Your post is very good.Following your posts.
Hi there, your post is perfect & few things are really updated. Following your website……
Hey! I would like to thank you for the efforts you’ve put in writing this site. Just wanted to say great site. Keep up the good work!