Jaundice : Significance, Production, Transportation, Metabolism & Laboratory Analysis
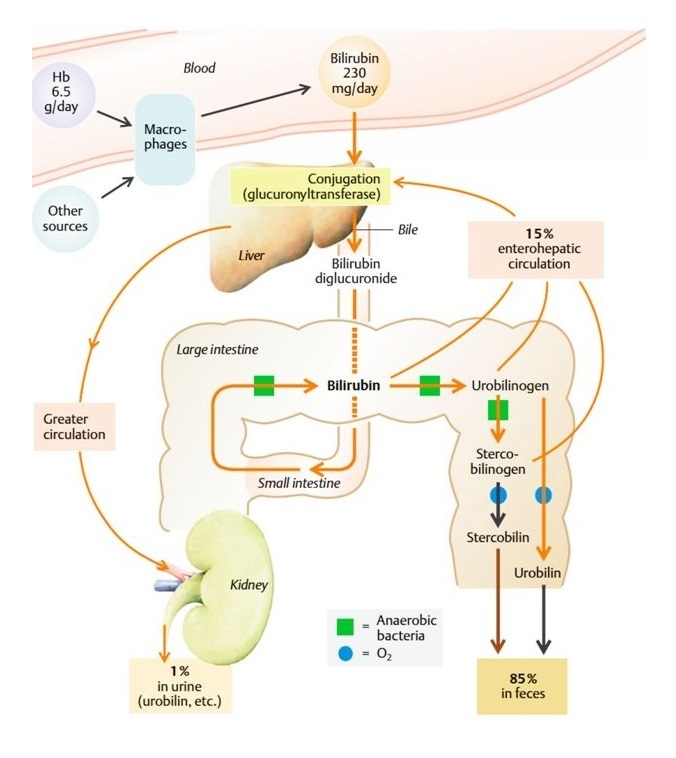
Bilirubin is formed from the breakdown of hemoglobin in the reticuloendothelial system; the end -products of heme catabolism are bilepigments. After breakdown of haemoglobin, the globin chains are separted, they are hydrolysed and the amino acid are channelled into the body amino acid pool. The iron liberated from heme is re-utilised. The Fe++ liberated is oxidised Fe++ and taken up by transferrin. The porphyrin ring is broken down in reticuloendothelial cells of liver, spleen and bone marrow to bile pigments; linear tetrapyrrole is biliverdin which is green in colour which is further reduced to bilirubin, a red-yellow pigment, by an NADPH dependent biliverdin reductase. About 6 gm of Hb is broken down per day and a total of 300 mg of bilirubin is formed every day from which about 250 mg of bilirubin is formed and 50 mg of bilirubin is formed from myoglobin and other heme containing proteins. About 80% is from destruction of old RBCs, 10% from ineffective erythropoiessis and the rest 10% from degradation of myoglobin and other heme containing proteins. Approximately 35 mg of bilirubin is formed from 1 gm of haemoglobin.
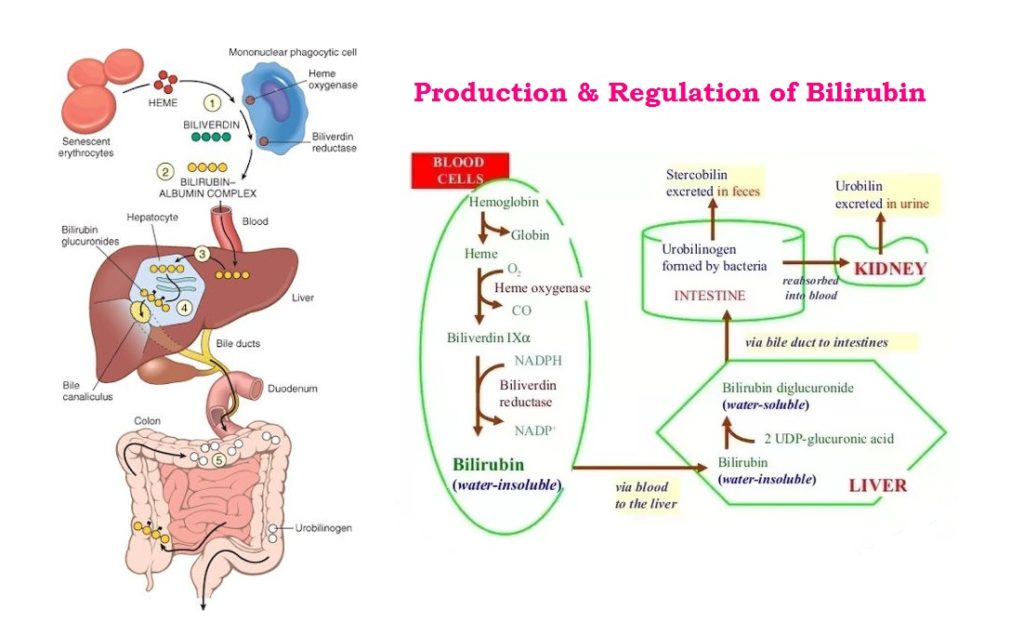
The liver plays the central role in the further disposal of the bilirubin. The indirect bilirubin bound to serum albumin gets transported through the blood to the liver. The free unconjugated bilirubin or indirect bilirubin is insoluble in water, cannot be filtered through the glomerulus. In the liver, bilirubin is removed by parenchymal cells. One molecule of albumin can bind 2 molecules of bilirubin. 100 ml of plasma can transport upto 25 mg of bilirubin. It is converted to water soluble conjugated bilirubin or direct bilirubin by the action of enzyme glucuronyl transferase, by conjugation with glucuronic acid. Drugs like primaquine, novobiocin, chloram-phenicol, androgens and pregnanediol may interfere in this conjugation process and may cause jaundice. This, conjugated bilirubin is excited by the liver through the bile duct and into the duodenum. In the intestine, bilirubin is converted by bacterial enzymes to several related compounds, collectively called as urobilinogen. Most of urobilinogen is lost in feces as stercobilinogen; after exposure to air as strecobilin. Urobilinogen and Stercobilinogen are both colourless compounds but are oxidised to coloured products, urobilin or stercobilin respectively by atmospheric oxidation. Urobilin is present in both the specimen, urin as well as in feces. About 10 to 15% of urobilinogen is reabsorbed into the blood stream and returns to liver by portalblood. Conjugated bilirubin is not bound to protein, it is easily filtered through the glomerulus and reexcreted in the intestine and through the kidney as a composition of urine. Excretion rate is 1 to 4 mg in 24 hrs., freshly collected normal urine usually gives positive reaction urobilinogen. Normally very small concentration 0.2-0.4 mg/dl of conjugated bilirubin is present in blood due to regurgitation, back from the bileduct.
Normal plasma bilirubin level ranges from 0.2- 1.0 mg/dl. The unconjugated bilirubin is about 0.2-0.6 mg/dl , while conjugated bilirubin is only 0-0.2 mg/dl. If the plasma bilirubin level exceeds 1 mg/dl, the condition is called hyperbilirubinemia. Levels between 1 and 2 mg/dl are indicative of latent jaundice. When the bilirubin level exceeds 2 mg/dl, It diffuses into tissues producing yellowish discolouration of sclera,conjunctiva, skin and mucous membrane resulting in jaundice or Icterus (Greek term for jaundice).
The estimation of direct and indirect bilirubin may help in the differential diagnosis of various types of jaundice; pre-hepatic, hepatic and post-hepatic.
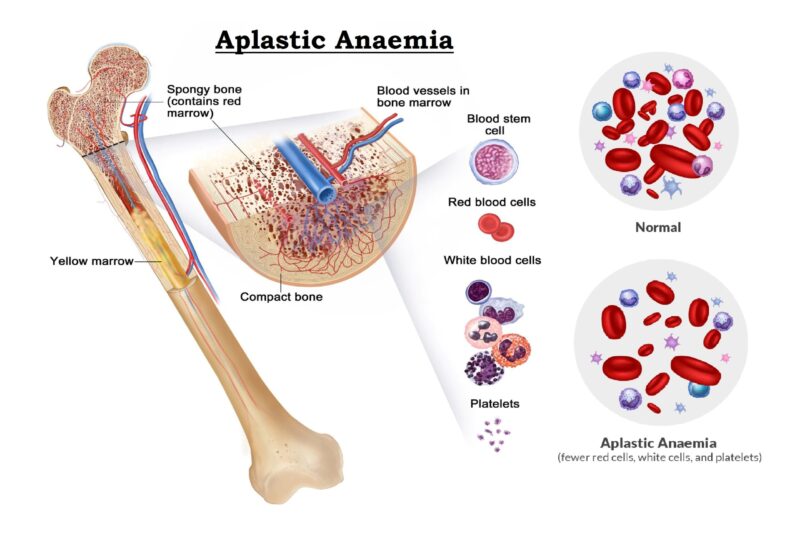
- Pre-hepatic jaundice : In Pre-hepatic jaundice the unconjugated bilirubin is increased due to the increase destruction of red cells, and the normally functioning liver is unable to cope with the incresed demand for cojugation. Hence there is an increase in unconjugated biliubin while conjugated bilirubin is normal. here no bilirubin will be excreted in the urine because unconjugated bilirubin cannot be filtered at the glomerulus. Due to the increased formation of unconjugated bilirubin, the rate of formation of urobilinogen increases considerably and it is excreted in urine in high proportion. The diseases related to pre-hepatic conditions are sickle cell disease, thalassemia major, acquired hemolytic anaemia due to leukemias, carcinoma etc., Hereditary spherocytosis, Glucose-6-phosphate dehydrogenase (G-6-PD) deficiency associated with drugs such as aspirin, sulfonamides & anti-malarial, infections like malaria, septicemia, physical agents like burns and incompatible blood transfusion etc.
- Hepatic Jaundice : In hepatic conditions, the conjugation of bilirubin is disturbed due to liver disorder, as a result the excretion of bilirubin is greatly decreased. Following the non-passage of bilirubin through the liver, the concentration of total bilirubin increases in the blood. The clinical picture varies according to the type & degree of hepatic injury. In viral hepatitis, specially cirrhosis of liver with hepatitis there may be injury to the parenchymal cells of the liver. In case of chemical intoxication or drug reaction (intrahepatic disease); the flow of conjugated bilirubin into the duodenum is inhibited and the bilirubin backs up in blood and excreated through the urine. Although incase of partial intrahepatic obstrction, bilirubin in higher concentration is still able to pass into the intestine and the rate of formation of urobilinogen increase which is excreted in urine in moderately increased proportion.
- Post-hepatic Jaundice : Post-hepatic conditions are related to an obstruction in the common bile duct caused by gallstones, carcinoma, pancreatitis or diseased lymph nodes surrounding that duct. The obstruction prevents the entry of bilirubin into the duodenum; hence the bilirubin backs-up into the blood, which causes jaundice. In this case, bilirubin is unable to get into the intestine, urobilinogen cannot be formed. It may be absent in urine and the feces will have a characteristic grey-white appearance and conjugated water soluble bilirubin is excreated through the urine.
Physiological Jaundice :
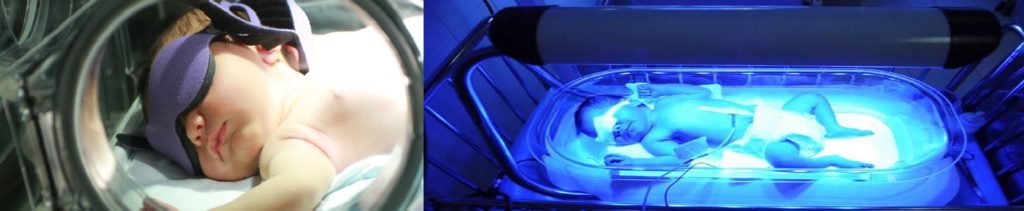
The most commonly occurring form of unconjugated hyperbilirubinemia is seen in Neonates. Normally newborns have serum unconjugated bilirubin concentrations greater than the healthy normal adults population. About 50% of the newborn population is clinically jaundiced during the first 5 days of life. In the normal fullterm neonate, unconjugated bilirubin levels raise upto 4-5 mg/dl and some time it’s goes upto 10 mg/dl within 48 hours afterwards decrease to normal levels in 7 to 10 days. This temporary increase of unconjugated bilirubin is caused by an increase bilirubin production as a result of haemolysis of erythrocytes and incomplete mutation of bilirubin metabolism and excretion. If the unconjugated bilirubin level exceeds 17 – 20 mg/dl in fullterm infant, there is a risk of Kernicterus (serum bilirubin enter the brain through crossing blood brain barrier & damage of brain). Infant with neonatal jaundice treated by applying Phototherapy (colour light application), which works by converting the water insoluble unconjugated bilirubin to water soluble cis-bilirubin isomer (Trans-bilirubin conversation). The principle of phototherapy is based on an application of a specific frequency of blue light. The light can be applied on the baby’s body surface with a overhead lamps but the baby’s eyes need to be covered by a Biliblanket, which placed under the baby’s cloth.
Determination of Serum Bilirubin
The most widely used methods for the determination of bilirubin are based on the diazo reaction, which was described by Ehrlich in 1883. In diazo reaction, diazotized sulfanilic acid (diazo reagent) reacts with bilirubin to produce reddish purple at natural pH and blue colour at low or high pH values due to formation of two azodipyrroles. In 1916, Van den Bergh and Muller applied this reaction for the quantitative determination of serum bilirubin . They found out that alcohol accelerated the diazo reaction of unconjugated bilirubin . This investigation describe that the bilirubin reacts with diazo reagent to produce coloured azo pigment. At acidic pH (pH 5), the pigment is purple in colour and the conjugated bilirubin being water soluble gives the colour immediately; hence called direct reaction. Whereas unconjugated bilirubin requires an accelerator or solubilizer, such as alcohol and it has to be extracted first with alcohol afterwards the reaction becomes positive; hence called indirect reaction. Total bilirubin is the added value of both conjugated and Unconjugated bilirubins.
Method :
Malloy & Evelyn
Principle :
- Direct Bilirubin : Bilirubin couples with diazotized sulfanilic acid, forming Azo-bilirubin, a red-purple colored product in acidic medium.
- Indirect Bilirubin : Bilirubin is diazotized only in the presence of its dissolving solvent (methanol). Thus the red purple colored Azobilirubin produced in presence of methanol originates from both Direct and Indirect fractions and represents Total Bilirubin concentrations. The difference of Total and Direct Bilirubin gives Indirect Bilirubin.
- The intensity of the produced red-purple colour is measured colourimetrically at 540 nm (green filter) and it’s directly proportional to the concentration of the appropriate fraction of bilirubin present in the specimen.
- Bilirubin +Diazotized Sulfanilic acid – Azobilirubin (Red-purple color)
Specimen :
Although Serum is preferred for enzymatic assay, heparinized plasma can also be used (free from haemolysis). The serum specimen for bilirubin determination should be used immediately as far as possible on the same day, if not tested immediately store the specimen in an amber coloured bottle at 2-8°C for not more than 24 hours. Gross contamination at any stage makes the specimen unsuitable for bilirubin determination. The samples should be brought to room temperature before use. No prior patient preparation is needed.
Reagent :
- Reagent 1 : Diazo A
- Reagent 2 : Diazo B
- Reagent 3 : Diazo Blank
- Reagent 4 : Methanol
- Reagent 5 : Artificial standard (10 mg % Bilirubin)
Just before use mix 1.0 ml of Reagent 1 with 0.030 ml of Reagent 2.
Procedure :
- All the reagents are brought to the room temperature before the test.
- Four dry and clean Test tubes are taken and marked these Test tubes properly as Direct (D1), Direct Blank (D2), Total (T1) and Total Blank (T2).
- Prepare separate Blank (T2 and D2) for each sample to be assayed.
- Dispense the Diazo reagent, Distilled water, Diazo Blank, Serum and Methanol in the above mention test tube respectively.
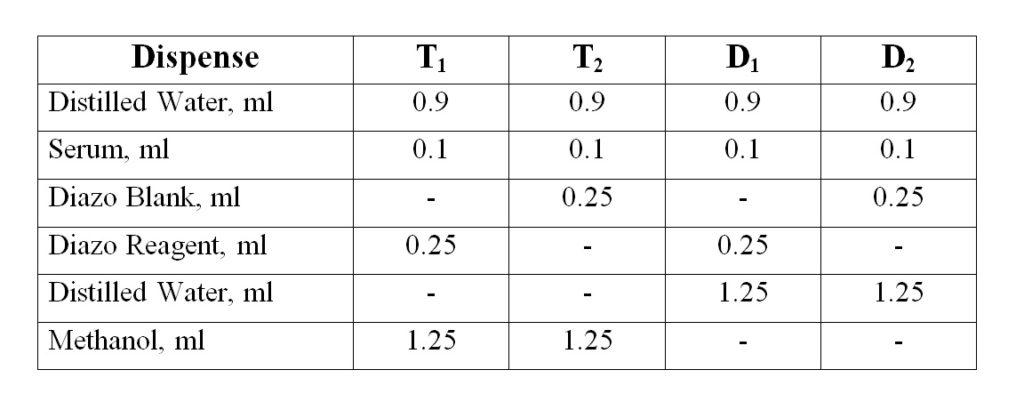
- Mixed well and keep the tubes T2 and T1 in dark at room temperature for 30 minutes and read the absorbance [Optical Density (OD)] of Test and Standard against Distilled water in the Colorimeter at 540 nm (green filter) and give the result as mg/dl.
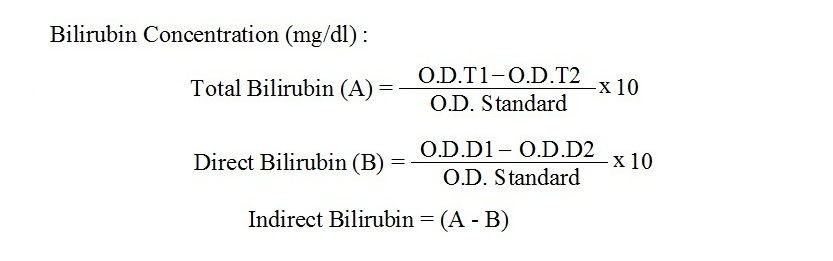
- Calculation :
Special Attention :
- A morning blood sample (preferably for serum) from a fasting personnel is preferred to avoid lipemia. Haemolysis of the serum specimen should be avoided since it produces falsely low values with Diazo methods (Haemolysis inhibits diazo reaction).
- Both Conjugated and Unconjugated bilirubin are photo-oxidized when exposed to white or UV-light. Specimen should be protected from direct exposure to either artificial light or sunlight as soon as they are drawn. Exposure to light decreases bilirubin level in the serum specimen.
- Storage of specimens in the dark and at low temperature is essential 2-8°C in the refrigerator.
- The method is linear upto 20 mg/dl. If serum bilirubin level is > 20 mg/dl then dilute the specimen & repeat the test. Apply proper dilution factor for the calculation of final result.



Hey there , You’ve done an excellent job. I will definitely digg it and personally suggest to my friends. I’m confident they will be benefited from this website. All is going well here and of course every one is sharing facts, that’s truly fine, Great work, keep up writing…
Hallo, You are actually a good Writer.
Studying and learning from your website is really nice. Thank you, keep writing…..