Hepatitis C : Sign & Symptoms, Transmission, Risk factors, Diagnosis, Complication, Treatment and Prevention
Hepatitis C is a viral infection caused by the hepatitis C virus that causes liver inflammation, sometimes leading to serious liver damage. The infection spreads when blood contaminated with the virus enters the bloodstream of an uninfected person; hence it's also called TTI (Transfusion Transmitted Infection). Hepatitis C can range from a mild illness lasting a few weeks to a serious, lifelong illness. Hepatitis C is often described as “acute,” meaning a new infection or “chronic,” meaning lifelong infection. Acute hepatitis C occurs within the first 6 months after someone is exposed to the hepatitis C virus. Hepatitis C can be a short-term illness, but for most people, acute infection leads to chronic infection. Chronic hepatitis C can be a lifelong infection with the hepatitis C virus if left untreated. Left untreated, chronic hepatitis C can cause serious health problems, including liver damage, cirrhosis (scarring of the liver), liver cancer, and even death.
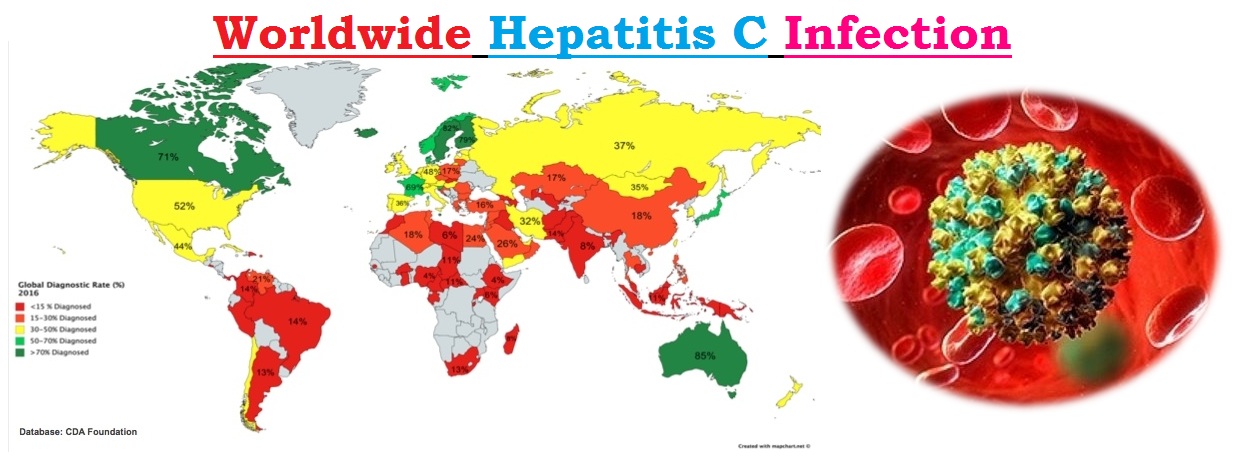
Globally, an estimated 71 million people have chronic hepatitis C virus infection. A significant number of those who are chronically infected will develop cirrhosis or liver cancer. WHO estimated that in 2016, approximately 399 000 people died from hepatitis C, mostly from cirrhosis and hepatocellular carcinoma (primary liver cancer). Antiviral medicines can cure more than 95% of persons with hepatitis C infection, thereby reducing the risk of death from cirrhosis and liver cancer, but access to diagnosis and treatment is low. There is currently no effective vaccine against hepatitis C; however, research in this area is ongoing. Worldwide, HCV exists in several distinct forms, known as genotypes. The most common HCV genotype in North America and Europe is type 1. Type 2 also occurs in the United States and Europe, but is less common than type 1. Both type 1 and type 2 have also spread through much of the world, although other genotypes cause a majority of infections in the Middle East, Asia and Africa. Although chronic hepatitis C follows a similar course regardless of the genotype of the infecting virus, treatment recommendations vary depending on viral genotype.
Sign & Symptoms
The incubation period for hepatitis C ranges from 2 weeks to 6 months. Following initial infection, approximately 80% of people do not exhibit any symptoms. Those who are acutely symptomatic may exhibit fever, fatigue, decreased appetite, nausea, vomiting, abdominal pain, dark urine, grey-coloured faeces, joint pain and jaundice (yellowing of skin and the whites of the eyes).Long-term infection with the hepatitis C virus (HCV) is known as chronic hepatitis C. Chronic hepatitis C is usually a "silent" infection for many years, until the virus damages the liver enough to cause the signs and symptoms of liver disease. Among these signs and symptoms are:
-
- Bleeding easily
- Bruising easily
- Fatigue
- Poor appetite
- Yellow discoloration of the skin and eyes (jaundice)
- Dark-colored urine.
- Itchy skin.
- Fluid buildup in your abdomen.
- Swelling in your legs.
- Weight loss.
- Confusion, drowsiness and slurred speech (hepatic encephalopathy).
- Spider-like blood vessels on the skin (spider angiomas).
- Every chronic hepatitis C infection starts with an acute phase. Acute hepatitis C usually goes undiagnosed because it rarely causes symptoms. When signs and symptoms are present, they may include jaundice, along with fatigue, nausea, fever and muscle aches. Acute symptoms appear one to three months after exposure to the virus and last two weeks to three months.
- Acute hepatitis C infection doesn't always become chronic. Some people clear HCV from their bodies after the acute phase, an outcome known as spontaneous viral clearance. In studies of people diagnosed with acute HCV, rates of spontaneous viral clearance have varied from 14 to 50 percent. Acute hepatitis C also responds well to antiviral therapy.
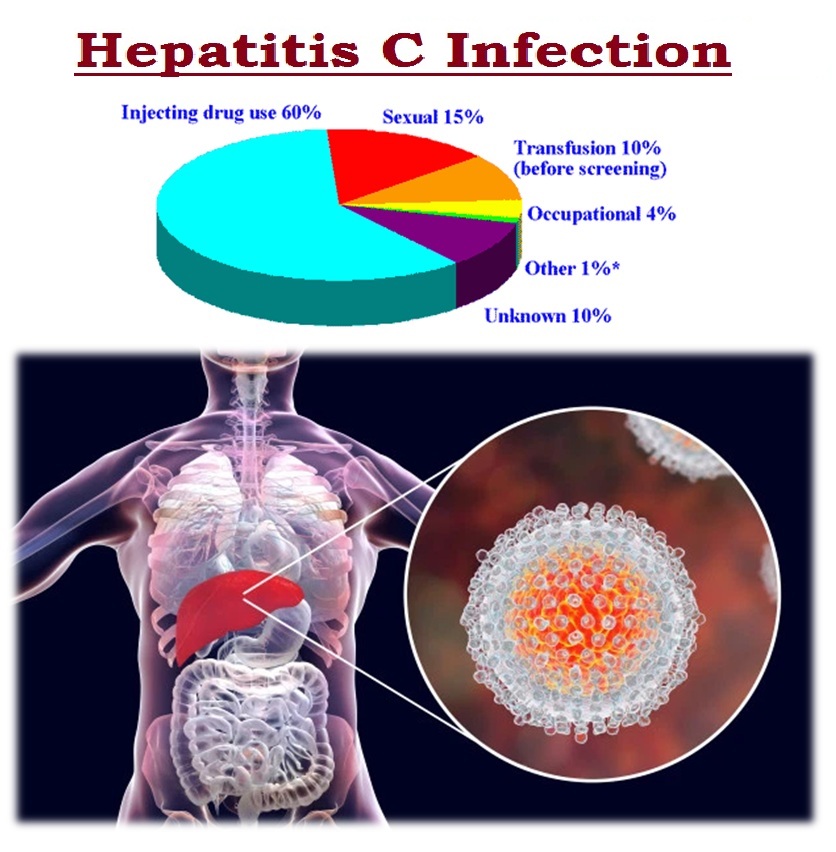
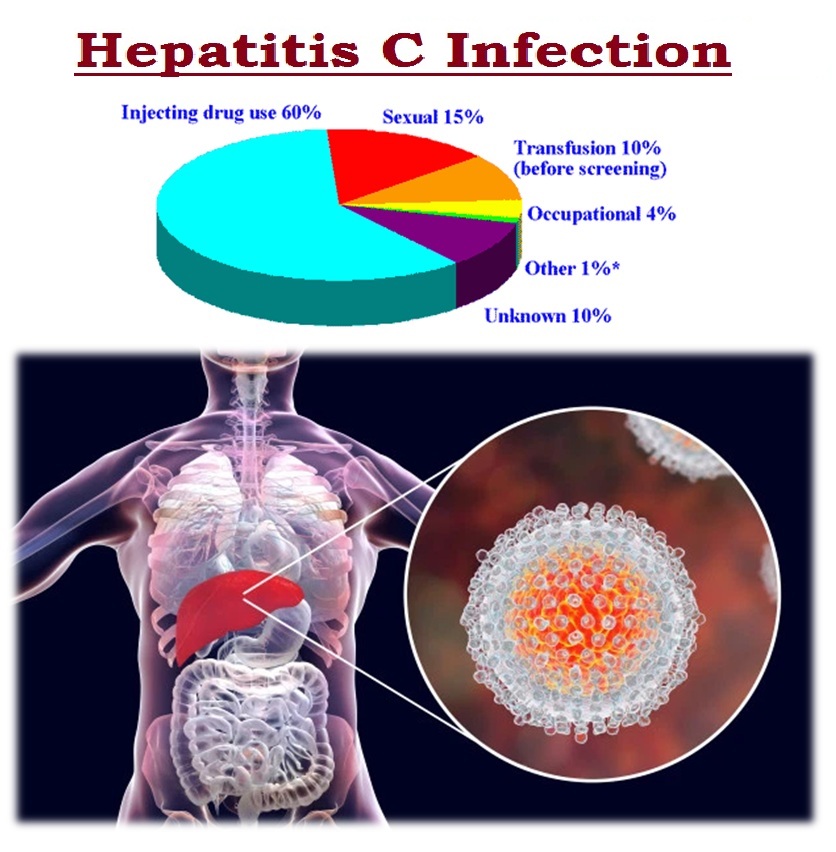
Mode of Transmission
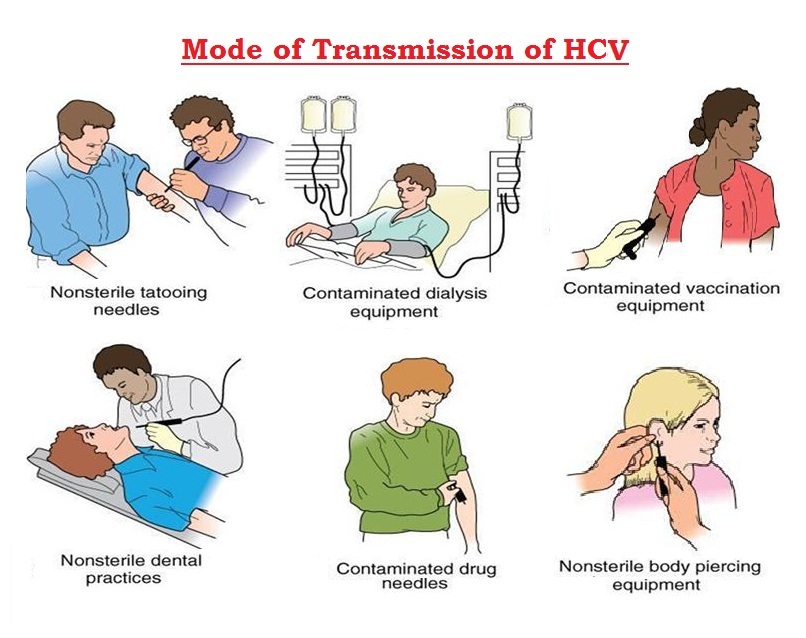
The hepatitis C virus is a bloodborne virus. It is most commonly transmitted through injecting drug use through the sharing of injection equipment, the reuse or inadequate sterilization of medical equipment, especially syringes and needles in healthcare settings, the transfusion of unscreened blood and blood product and/or sexual practices that lead to exposure to blood (for example, among men who have sex with men, particularly those with HIV infection or those taking pre-exposure prophylaxis against HIV infection).
HCV can also be transmitted sexually and can be passed from an infected mother to her baby; however, these modes of transmission are less common.
Hepatitis C is not spread through breast milk, food, water or casual contact such as hugging, kissing and sharing food or drinks with an infected person.
WHO estimates that in 2015, there were 1.75 million new HCV infections in the world (23.7 new HCV infections per 100 000 people).
Risk factors
Risk of hepatitis C infection is increased if the patients:
-
- Are a Healthcare worker who has been exposed to infected blood, which may happen if an infected needle pierces patient's skin.
- Have ever injected or inhaled illicit drugs.
- Have HIV infection.
- Create a piercing or tattoo in an unclean environment using unsterile equipment.
- Received a blood transfusion or organ transplant before 1992.
- Received clotting factor concentrates before 1987.
- Under hemodialysis treatments for a long period of time.
- Were born to a woman with a hepatitis C infection.
- Were ever in prison.
- Were born between 1945 and 1965, the age group with the highest incidence of hepatitis C infection.
Diagnosis of Hepatitis C
Healthcare officials recommend that anyone at high risk of exposure to HCV get a blood test to screen for hepatitis C infection. People who may want to talk to their doctors about screening for hepatitis C include:
-
- Anyone who has ever injected or inhaled illicit drugs.
- Anyone who has abnormal liver function test results with no identified cause.
- Babies born to mothers with hepatitis C.
- Healthcare and emergency workers who have been exposed to blood or accidental needle sticks.
- People with hemophilia who were treated with clotting factors before 1987.
- Patient who have ever undergone long-term hemodialysis treatments.
- People who received blood transfusions or organ transplants before 1992.
- Sexual partners of anyone diagnosed with hepatitis C infection.
- People with HIV infection.
- Anyone born from 1945 to 1965.
- Anyone who has been in prison
- Other Blood Tests : If an initial blood test shows that you have hepatitis C, additional blood tests will:
- Measure the quantity of the hepatitis C virus in your blood (viral load)
- Identify the genotype of the virus
- Tests for Liver Damage : Doctors typically use one or more of the following tests to assess liver damage in chronic hepatitis C infection.
- Magnetic resonance elastography (MRE) : A noninvasive alternative to a liver biopsy (see below), MRE combines magnetic resonance imaging technology with patterns formed by sound waves bouncing off the liver to create a visual map showing gradients of stiffness throughout the liver. Stiff liver tissue indicates the presence of fibrosis, or scarring of the liver, as a result of chronic hepatitis C.
- Transient elastography : Another noninvasive test, transient elastography is a type of ultrasound that transmits vibrations into the liver and measures the speed of their dispersal through liver tissue to estimate its stiffness.
- Liver biopsy : Typically done using ultrasound guidance, this test involves inserting a thin needle through the abdominal wall to remove a small sample of liver tissue for laboratory testing.
- Transient elastography : A member of the care team performs transient elastography — a painless alternative to liver biopsy — to assess liver damage.
Complications
Hepatitis C infection that continues over many years can cause significant complications, such as:
-
- Scarring of the liver (cirrhosis) : After 20 to 30 years of hepatitis C infection, cirrhosis may occur. Scarring in the liver makes it difficult for the liver to function.
- Liver cancer : A small number of people with hepatitis C infection may develop liver cancer.
- Liver failure : Advanced cirrhosis may cause the liver to stop functioning.
Treatment
- Antiviral Medications : Hepatitis C infection is treated with antiviral medications intended to clear the virus from the body. The goal of treatment is to have no hepatitis C virus detected in the body at least 12 weeks after the complete treatment. Researchers have recently made significant advances in treatment for hepatitis C using new, "direct-acting" anti-viral medications, sometimes in combination with existing ones. As a result, people experience better outcomes, fewer side effects and shorter treatment times — some as short as eight weeks. The choice of medications and length of treatment depend on the hepatitis C genotype, presence of existing liver damage, other medical conditions and prior treatments. Due to the pace of research, recommendations for medications and treatment regimens are changing rapidly. It is therefore best to discuss your treatment options with a specialist. Throughout treatment your care team will monitor the response to medications.
- Liver Transplantation : If the patient have developed serious complications from chronic hepatitis C infection, liver transplantation may be an option. During liver transplantation, the surgeon removes your damaged liver and replaces it with a healthy liver. Most transplanted livers come from deceased donors, though a small number come from living donors who donate a portion of their livers. In most cases, a liver transplant alone doesn't cure hepatitis C. The infection is likely to return, requiring treatment with antiviral medication to prevent damage to the transplanted liver. Several studies have demonstrated that new, direct-acting antiviral medication regimens are effective at curing post-transplant hepatitis C. Treatment with direct-acting antivirals can also be effective in appropriately selected patients before liver transplantation.
- Vaccinations : Although there is no vaccine for hepatitis C, Doctor will likely recommend that receive vaccines against the hepatitis A and B viruses. These are separate viruses that also can cause liver damage and complicate the course of chronic hepatitis C.
Prevention of Hepatitis C infection
There is no effective vaccine against hepatitis C, therefore prevention of HCV infection depends upon reducing the risk of exposure to the virus in health-care settings and in higher risk populations. Protect from hepatitis C infection by taking the following precautions:
-
- Stop using illicit drugs, particularly if inject them. If use illicit drugs, seek help.
- Be cautious about body piercing and tattooing. If choose to undergo piercing or tattooing, look for a reputable shop. Ask questions beforehand about how the equipment is cleaned. Make sure the employees use sterile needles. If employees won't answer questions, look for another shop.
- Practice safer sex. Don't engage in unprotected sex with multiple partners or with any partner whose health status is uncertain. Sexual transmission between monogamous couples may occur, but the risk is low.
- Education and counselling on options for care and treatment.
- Immunization with the hepatitis A and B vaccines to prevent coinfection from these hepatitis viruses and to protect their liver.
- Early and appropriate medical management including antiviral therapy and regular monitoring for early diagnosis of chronic liver disease.


Like!! Great article post.Really thank you! Really Cool.
It’s actually a great and helpful piece of information. I am glad that you shared this helpful info with us. Please keep us informed like this. Thanks for sharing.